Prevalence of Depression among Resident Doctors in King Fahad Medical City, Riyadh, Saudi Arabia
Othman Majed Alothman*, Yazzan Mohammed Alotaibi, Sulaiman Ibrahim Alayed, Saleh Khalid Aldakhil, Mohammed Abdullah Alshehri
Faculty of Medicine, Imam Mohammad Ibn Saud Islamic University, Riyadh, KSA.
*Email: othman.alothman96 @ gmail.com
ABSTRACT
Background: Depression is a common mental disorder in adults, and the World Health Organization (WHO) has ranked it as the fourth leading cause of disability worldwide. Doctors are not immune to the disorder; in fact, they have a higher risk than the general population, which affects the physician’s life and compromises the quality of the health services. In Saudi Arabia, resident doctors’ mental health is under-recognized, and more studies need to be conducted to fill this gap. Objectives: This study is aimed at determining the prevalence of depression among resident doctors working at a tertiary care hospital in Riyadh, and analyzing the associated factors. Methodology: The study utilized a cross-sectional design. The resident doctors in KFMC hospital in Riyadh participated in this study by filling questionnaires, including a depression-screening instrument (CES-D), a sociodemographic datasheet, and questions about other associated factors. Results: One hundred and nineteen residents responded with an overall response rate of 70%. Based on categorical levels of the CES-D, 41% (49) did not have depression, 20% (24) had mild to moderate depression, and 39% (46) had probable major depression. There were significant differences in depression by gender with higher rates among women (55.1%) than men (27.1%). Further, participants with a history of depression were more likely to have depression (62%).
Key words: Mental health, Riyadh, Doctors, Depression, Saudi Arabia.
INTRODUCTION
Depression is a common mental disorder characterized by depressed mood, fatigue, social withdrawal, and an inability to perform everyday functions for at least two weeks. In extreme cases, when left untreated, it may be accompanied by thoughts of death and suicide. The World Health Organization has ranked depression as the fourth leading cause of disability worldwide. In the United States alone, major depressive disorder (MDD) affects 14.8 million adults every year, and is one of the largest causes of disability, especially among women [1, 2]. The lifetime prevalence of depression is high [3-5]. While the cause of the disorder remains unknown, various risk factors, such as poverty, abuse, work stress, genetic makeup, and chemical imbalance, have been recognized as probable contributors [6].
Healthcare workers’ mental health has been an issue of concern for many years. Numerous studies have reported alarming rates of stress, depression, and burnout among healthcare workers, especially doctors and nurses. A 2015 study showed that 23% of health workers displayed depressive symptoms and 34% displayed high levels of distress [7, 8].
Depression among physicians is high as compared to other professionals, and it may even lead to suicide, which is a leading cause of death among medical students. The suicide rate among physicians is more than twice that of the general population. Depression not only affects the mental health of the physician but also causes physical problems. Research has shown that male physicians are at risk of myocardial infarction and immune suppression, conditions that have been linked to infectious diseases and cancer [9].
Stress and burnout, long working hours, taking difficult medical decisions, dealing with death, and massive amounts of workload, all may contribute to depressive symptoms during the residency period. Resident doctors have numerous duties, including attending to patients and studying course-related material, putting great amounts of pressure on them that may eventually lead to depression. Depression in resident doctors affects not only them, but it may spill over to negatively affect their patients as well as affecting their learning and academic pursuits, which are a crucial part of a medical postgraduate student’s life [10-14].
A 2015 meta-analysis of 54 studies involving 17560 physicians in training demonstrated that between 20.9% and 43.2% of trainees screened positive for depression or depressive symptoms during residency [15].
Studies on medical residents in different countries have shown high rates of depression during their training. For example, a study conducted in Turkey found that the prevalence rate of depression among resident doctors was 16.0% and that the rate of depression was significantly higher among women than men [16]. A more recent study conducted in Pakistan found that doctors showed high levels of anxiety and depression, and female doctors were more prone to anxiety than their male counterparts [17].
Research on the mental health of resident doctors is under-recognized, especially in Saudi Arabia, where only a few studies have been conducted on this subject. A recent study reported that resident doctors in Saudi Arabia are at a comparable or slightly higher risk of perceived stress than residents worldwide [18, 19]. The prevalence of depression among doctors in Saudi Arabia is unknown; however, some studies conducted among medical students have reported high rates of depression, as 17.8% of the 1171 participants had severe major depression and 17.8% had moderately severe depression [20].
The present study was conducted to screen for the prevalence of depression among resident doctors working at a tertiary care hospital in Riyadh, with a considerable focus on the associated sociodemographic factors. The study aims to fill the existing gap in knowledge regarding physicians’ mental health in Saudi Arabia, to draw attention to their current status, and highlight the need to look for solutions to this issue.
MATERIALS AND METHODS
The study followed a cross-sectional design, targeting resident doctors from all different specialties in KFMC, Riyadh. To be included in the study, participants had to be licensed resident doctors working in King Fahad Medical City.
The KFMC hospital research center provided a mailing list of the target population. Questionnaires were sent to the doctors, who fulfilled the aforementioned inclusion criteria, via an institution e-mail ID. The recipients were requested to fill and return the questionnaires within a week. The data were analyzed using IBM SPSS V24.
The Center for Epidemiological Studies-Depression (CES-D) scale was used to assess depression in the participants. This 20-item measure has a response range from zero (rarely or none of the time) to three (most or all of the time). Based on the positive predictive value, sensitivity, and specificity for depression, the following cutoff scores have been proposed for the CES-D: A score of less than 15 indicates no depression, 15-21 indicates mild to moderate depression, and over 21 indicates major depression.
The sociodemographic factors included site, trainee level, and gender. Besides, the participants were asked to answer the following yes/no questions: whether they had a history of depression and, if so, whether they had received treatment; whether they were currently receiving treatment for mental health issues; and whether they had a family history of depression.
The research IRB was approved by the King Fahad research center. All questionnaires included a consent form. Participation in the study was voluntary and all participants were ensured data privacy, anonymity, and confidentiality.
RESULTS
Out of the 170 individuals to whom the emails were sent, 119 responded (70%) with completed questionnaires. Of these, 58.8% were males. A majority of the participants were under 30 of age (86.6%). In total, 59.7% of the respondents were single, 37% were married, and 3.4% were divorced. Twenty percent of the respondents had a history of depression, of whom thirty-six had received treatment.
Figure 1 shows the prevalence of depression (using the CES-D scale) among the KFMC resident doctors, of whom 41% (49) did not have depression, 20% (24) had mild to moderate depression, and 39% (46) had probable major depression.
Table 2 shows that the prevalence of depression was slightly higher in participants over the age of 30. Females had a significantly higher rate of probable major depression (55.1%) than males (27.1%), whereas, males had a higher rate of mild to moderate depression (28.6%) than females (18.7%). Single participants had lower depression rates (54.9%) than divorced and married participants (75% and 63.6%, respectively). The married participants who had children had significantly higher rates of probable major depression than those who did not have children (75% and 32.2%, respectively).
There were no statistically significant differences by specialty and year of residency. However, the residents in the fourth-year or above were more likely to report experiencing depression. Moreover, the respondents with a history of depression were more likely to have probable major depression compared to those who did not have a history of depression (62% and 32.6%, respectively).
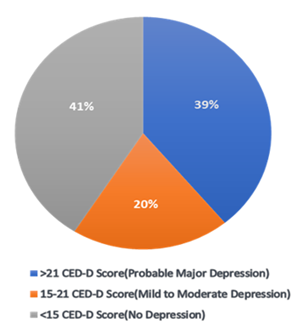
Figure 1: Prevalence of depression among resident doctors at KFMC (N=119)
Table 1. Sociodemographic and Work-life Characteristics of the Participants (n = 119).
|
Variable |
Frequency |
Percent |
|
Age (years) |
|
|
|
Under 30 |
103 |
86.60% |
|
30 and over |
16 |
13.40% |
|
Gender |
|
|
|
Male |
70 |
58.80% |
|
Female |
49 |
41.20% |
|
Marital status |
|
|
|
Married |
44 |
37% |
|
Single |
71 |
59.70% |
|
Divorced |
4 |
3.40% |
|
Presence of children |
|
|
|
Yes |
32 |
26.90% |
|
No |
87 |
73.10% |
|
Years of training |
|
|
|
PGY I |
43 |
36.10% |
|
PGY II |
27 |
22.70% |
|
PGY III |
18 |
15.10% |
|
PGY IV |
22 |
18.50% |
|
>PGY IV |
9 |
25.20% |
|
Specialty |
|
|
|
Neurology |
10 |
8.40% |
|
Pediatrics |
23 |
19.30% |
|
Gynecology |
3 |
2.50% |
|
Family medicine |
22 |
18.50% |
|
Neurosurgery |
6 |
5% |
|
Cardiac surgery |
2 |
1.70% |
|
Anesthesia |
11 |
9.20% |
|
Internal medicine |
17 |
14.30% |
|
Urology |
6 |
5% |
|
Radiology |
19 |
16% |
|
Number of ‘on-calls’ per month |
|
|
|
None |
25 |
21% |
|
1 – 5 |
75 |
63% |
|
6 –10 |
19 |
16% |
Table 2. Association between Sociodemographic Characteristics and Depression using CES-D Score among Resident Doctors at KFMC, Saudi Arabia.
|
Sociodemographic Characteristics |
Probable major depression (CES-D > 21) |
Mild to moderate depression (CES-D 15-21) |
No depression (CES-D < 15) |
P-Value |
|
Age (years) |
||||
|
Under 30 |
39 (37.9%) |
21 (20.4%) |
43 (41.7%) |
0.903 |
|
30 and over |
7 (43.7%) |
3 (18.7%) |
6 (37.5%) |
|
|
Gender |
||||
|
Male |
19 (27.1%) |
20(28.6%) |
31(44.3%) |
0.002 |
|
Female |
27 (55.1%) |
4(8.2%) |
18(36.7%) |
|
|
Marital status |
||||
|
Married |
19(43.2%) |
9(20.4%) |
16(36.4%) |
|
|
Single |
25(35.2%) |
14(19.7%) |
32(45.1%) |
0.839 |
|
Divorced |
2(50%) |
1(25%) |
1(25%) |
|
|
Presence of children |
||||
|
Yes |
18(75%) |
5(20.8%) |
9(4.2%) |
0.056 |
|
No |
28(32.2%) |
19(21.8%) |
40(46%) |
|
|
Years of training |
||||
|
PGY I |
12(27.9%) |
6(14%) |
25(58.1%) |
0.154 |
|
PGY II |
8(29.6%) |
8(29.6%) |
11(40.7%) |
|
|
PGY III |
9(50%) |
4(22.2%) |
5(27.8%) |
|
|
PGY IV |
13(59.1%) |
4(18.2%) |
5(22.7%) |
|
|
>PGY IV |
4(44.4%) |
2(22.2%) |
3(33.3%) |
|
|
Specialty |
||||
|
Neurology |
5(50%) |
2(20%) |
3(30%) |
0.5 |
|
Pediatrics |
13(56.5%) |
4(17.4%) |
6(26.1%) |
|
|
Gynecology |
2(66%) |
0(0%) |
1(33%) |
|
|
Family medicine |
6(27.3%) |
2(9.1%) |
14(63.6%) |
|
|
Neurosurgery |
2(33.3%) |
2(33.3%) |
2(33.3%) |
|
|
Cardiac surgery |
1(50%) |
0(0%) |
1(50%) |
|
|
Anesthesia |
3(27.3%) |
5(45.4%) |
3(27.3%) |
|
|
Internal medicine |
6(35.3%) |
4(23.5%) |
7(41.2%) |
|
|
Urology |
3(50%) |
1(16.7%) |
2(33.3%) |
|
|
Radiology |
5(26.3%) |
4(21%) |
10(52.6%) |
|
|
History of depression |
||||
|
Yes |
5(20.8%) |
4(16.7%) |
0.012 |
|
|
No |
31(32.6%) |
19(20%) |
45(47.4%) |
DISCUSSION
Resident doctors are exposed to a variety of work-related stresses that affect their productivity and mental health.
This study showed that 20% of the participant doctors had mild to moderate depression and 39% had probable major depression. These figures are higher than the prevalence reported by a similar study where 12% of participants had probable major depression and 9% had mild to moderate depression [21]. A study conducted in Turkey reported a probable depression rate of 16% using the Beck Depression Inventory (BDI) [16]. Another study in Pakistan reported a depression rate of 24.8% using the Hospital Anxiety and Depression Scale (HADS) [17]. The differences in the reported prevalence rates could be probed further and explained using a different measure of depression and larger sample size.
In the present study, we could not find a statistically significant association between the year of training and depression, which is consistent with previous research [16, 21]. Furthermore, both age and medical specialty had no significant association with the manifestation of depression. Women had a significantly higher rate of probable major depression compared to men, which is consistent with other studies [16, 21]. Additionally, the respondents who had a history of depression displayed a higher rate of depression than those who did not have a history of depression, which is comparable to a previous study [21]. Interestingly, the respondents who reported having children had a significantly higher rate of depression than those who did not have children.
A recent study conducted in Jeddah, Saudi Arabia revealed a high prevalence of depression among medical residents compared to previously conducted studies (mild depression was identified in 35.6%, and moderate to severe depression in 40.2% of the participants) [22].
Despite extensive global data, there have been minimal reports addressing depression among physicians in Saudi Arabia.
This study is limited by its cross-sectional nature, which limits the conclusions that can be drawn for causality. Further, we cannot rule out the possibility of a reporting bias arising from the self-reported nature of the data.
CONCLUSION
The main finding of this study is that more than half of the residents (59%) working at KFMC hospital reported having some degree of depression. Further, the data suggest that female residents should be evaluated as a high-risk group for depression, which indicates a need for preventive and control policies in work life. Whereas the doctors’ mental health should be a vital part of every health system, the rates of depression among resident doctors are concerning. There is a crucial need to address the disorder through effective interventions at both the individual and institutional levels. Professional counseling services to manage work-related stress, educational programs, and health promotion strategies are essential to improve the overall wellbeing of physicians. This study was limited to a major hospital in the urban city of Riyadh, which could have compromised the external validity of its results. Further multi-center studies are encouraged to get a more complete picture of the overall issue, determine the causes, and improve the work-related quality of life among medical residents.
REFERENCES
- World Health Organization. World Health Organization; [cited 2018Jul21]. Available from: http://www.who.int/.
- Beck AT. Depression / Aaron T: Beck. London: Staples. 1967.
- Ghaderi H, Rafieian M, Rahmani Nezhad H. Effect of Hydroalcoholic Cinnamomum Zeylanicum Extract on Reserpine-Induced Depression Symptoms in Mice. Pharmacophores. 2018; 9(2): 35-44.
- Ghaderi H, Nikan R, Rafieian-Kopaei M, Biyabani E. The Effect Of Cinnamon Zeylanicum Essential Oil On Treatment Of Patients With Unipolar Nonpsychotic Major Depressive Disorder Treated With Fluoxetine. Pharmacophores. 2017; 8(3): 24-31.
- Soh N H B C, Roy A. Stress, anxiety, and depression in clinical practice of undergraduates and awareness of its effective management -A survey. J. Adv. Pharm. Edu. Res. 2017; 7(2): 82-8
- What Is Depression? [Internet]. Mindfulness Practices May help Treat Many Mental Health Conditions. (cited 2018Jul21). Available from: https://www.psychiatry.org/patients-families/depression/what-is-depression.
- Ansoleaga E.: [Psychosocial stress among health care workers]. Rev Med Chil. 2015, 143(1):47-55.. 10.4067/S0034-98872015000100006.
- Depression and Dissatisfaction among Healthcare Workers. ([Psychosocial stress among health care workers].). Accessed: November 16, 2017: https://www.jonbarron.org/depression/depression-and-dissatisfaction-among-healthcare-workers.
- Physician Suicide: Overview, Depression in Physicians, Problems with Treating Physician Depression [Internet]. Background, Pathophysiology, Etiology. (2018). https://emedicine.medscape.com/article/806779-overview.
- Ogawa R, Seo E, Maeno T, Ito M, Sanuki M, Maeno T: The relationship between long working hours and depression among first-year residents in Japan. BMC Medical Education. 2018, 18: 50. 18
- Pauline Anderson. (Physicians Experience Highest Suicide Rate of Any Profession [Internet]. Medscape). https://www.medscape.com/viewarticle/896257.
- Tyssen R, Vaglum P: Mental Health Problems among Young Doctors: An Updated Review of Prospective Studies. Harvard Review of Psychiatry. 2002, 10(3):154-65. 10.1080/10673220216218
- Firth-Cozens J: Interventions to improve physicians’ well-being and patient care. Social Science & Medicine. 2001, 52:215-22. 10.1016/s0277-9536(00)00221-5
- Fahrenkopf AM, Sectish TC, Barger LK: Rates of medication errors among depressed and burnt out residents: prospective cohort study. 2008Jul, 336:488-91.12. 10.1136/bmj.39469.763218.BE
- Douglas A. Mata, MD, MPH1; Marco A. Ramos, et al.: Prevalence of Depression and Depressive Symptoms among Resident Physicians. 2015, 314(22):2373-2383. 10.1001/jama.2015845
- Demir F, Ay P, Erbaş M, Ozdil M, Yaşar E: [The prevalence of depression and its associated factors among resident doctors working in a training hospital in Istanbul]. [Internet]. Advances in pediatrics. U.S. National Library of Medicine. 2007 [cited 2018Jul21].
- Atif K, Khan HU, Ullah MZ, Shah FS, Latif A: Prevalence of anxiety and depression among doctors; the unscreened and undiagnosed clientele in Lahore, Pakistan. 2016, 32(2):294-8. 10.12669/pjms.322.8731
- Alosaimi F, Kazim S, Almufleh A, Aladwani B, Alsubaie A: Prevalence of stress and its determinants among residents in Saudi Arabia. Saudi Medical Journal. 2015Jan, 36:605-12. 10.15537/smj.2015.5.10814
- Mousa OY, Dhamoon MS, Lander S, Dhamoon AS: The MD Blues: Under-Recognized Depression and Anxiety in Medical Trainees. 2016, 10.1371/journal.pone.0156554
- Alsalameh NS, Alkhalifah AK, Alkhaldi NK: Depression among Medical Students in Saudi Arabia. . Egyptian Journal of Hospital Medicine. 2017, 68:974-81.
- Goebert D, Thompson D, Takeshita J, et al.: Depressive Symptoms in Medical Students and Residents: A Multischool Study. Academic Medicine. 2009, 84:236 41. 10.1097/acm.0b013e31819391bb
- Alshardi, A., Farahat, F. Prevalence and Predictors of Depression among Medical Residents in Western Saudi Arabia. J Clin Psychol Med Settings (2019). https://doi.org/10.1007/s10880-019-09667-7.
