Role of Cone-Beam Computed Tomography in the Detection of Maxillary Sinus Disease
Hanadi Sabban 1*, Ibrahim Yamany 2
1 Assistant professor of Oral and Maxillofacial Radiology, BDs, MDS, American Board, Diplomate of AOMFR, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia.
2 Associate professor of Oral and Maxillofacial Radiology, BDs, MDS, American Board, Diplomate of AOMFR, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia.
*Email: Hsabban @ kau.edu.sa
ABSTRACT
Dentists must understand the role of maxillary sinus diseases and their relationship to teeth and supporting structures. The most maxillary sinus disease is Odontogenic maxillary sinusitis. Cone-beam computed tomography (CBCT) is the imaging choice in dental practice to evaluate maxillary sinuses and maxillofacial structures. Maxillary sinuses carry a variation of mucosal thickening. If the mucosa of maxillary sinuses exceeds more than 2 mm, it indicates the possibility of infection in the maxillary sinuses. More than 50% of patients visiting the dental practice have thickening of lining mucosa more than 2 mm. Limitation for CBCT includes difficulty to differentiate between soft-tissue attenuation. This review aims to emphasize the role of CBCT in the detection of maxillary sinus diseases in dental practice. In conclusion, the CBCT examination is the best and convenient imaging tool in the dental practice that can identify the presence of pathology in maxillary sinus before surgery or post-operative complication and follow-up. This literature review was done to emphasize the demand for CBCT as an imaging investigation tool. This imaging modality is increased nowadays due to its accurate diagnosis of dental disease and routine evaluation of alveolar bone for implant placement and sinus lift surgery.
Key words: cone-beam computed tomography (CBCT), 3D radiography, maxillary sinus disease, odontogenic sinusitis, mucositis.
INTRODUCTION
CBCT has now become popular with clinicians because of its ability to image structures three-dimensionally and at the same time to visualize both bony and soft tissue structures with extremely thin section high-resolution images [1-3]. The dentist needs to understand the role of direct contact between the maxillary sinuses and the posterior maxillary teeth [4]. It is well known that maxillary dental infections can cause sinusitis. Chronic disease of teeth due to caries, trauma, or any local factor could reach the periapical tissue and cause odontogenic sinusitis, abscess, or oro-antral fistula [5, 6]. Forty percent of chronic bacterial maxillary sinus infections are attributed to a dental source. The origin of the site of infection in sinusitis can be effectively determined with accuracy and precision using CBCT and a fairly low dose of radiation. Sinusitis of odontogenic origin, radiographically appear as soft tissue density mass within the sinuses, originating from a carious tooth with a defective restoration, or an extraction site with or without a radiographically evident periapical lesion and mucosal thickening limited to the area of the tooth or extraction site in question. Conventional radiography has a limited view of maxillary sinuses while cone-beam computed tomography (CBCT) allows a 3-dimensional view of maxillary sinuses. This helps to understand the relationship between dental disease and maxillary sinus changes [7, 8]. This review is an attempt to make the general dentist aware of the role of CBCT in the identification of maxillary sinus diseases. Further, it will be useful to correlate sinus pathology with dental disease.
Clinical Significance
This literature review is highlighting the demand for CBCT as an imaging investigation tool for detecting maxillary sinus disease. Since CBCT is used routinely nowadays due to its accurate diagnosis of dental disease and evaluation of alveolar bone for implant placement and sinus lift surgery, dentists should investigate the presence of sinus pathology in advance to complete treatment for dental disease [9].
Maxillary sinuses and dental diseases
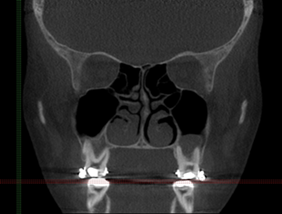
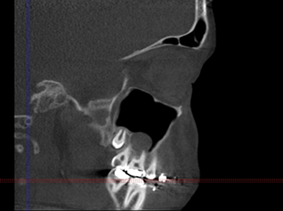
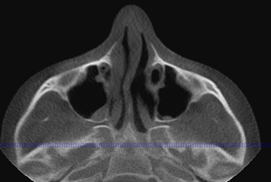
One of the most relevant anatomical structures in the maxilla, which are in direct proximity with the oral cavity is the maxillary sinuses. There are a pair of maxillary sinuses in maxilla which is connected to the nasal cavity with osteo-meatal complex. The palate bone represents the same anatomical structure of the maxillary sinus floor. See figure 1. [10]. The Schneiderian membrane is the lining membrane of maxillary sinus walls whose changes suggest sinus disease [11]. See figure 2.

Figure 1: CBCT scan, Coronal view, shows clear normal maxillary sinuses. Bilateral Radiolucent areas are representing maxillary sinuses. The nasal septum is deviated to right slightly.

Figure 2: Mucositis: thickening of lining mucosa (Schneiderian membrane)
Pneumatization is the enlargement of the sinus cavity with unknown etiology amongst the population. It is a metabolic process that takes place mostly between 12 years to 20 years old and then slowing process will take place due to the extraction of posterior dentition and migration of teeth [11-13]. Therefore, when severe cases of ridge atrophy are combined with pneumatization of maxillary sinuses due to the absence of maxillary teeth, a thin alveolar bone is present between the sinus floor and oral cavity [14]. See Figures 3 (A and B).
 |
 |
|
(A) |
(B) |
Figure 3: CBCT scan, (A) to the left is Coronal view, and (B) to the right is Sagittal view showing mucosal thickening of the inferior wall of the left maxillary sinus. Severe pneumatization of maxillary sinuses. The alveolar bone of maxilla is thin. The mild nasal septum has deviated to the left
The mucosal lining of the maxillary sinuses is similar to those lining the nasal cavity, but it has fewer numbers of mucous glands. The inner side of the lining mucosa contains the cilia which is responsible for washing the mucosal drainage toward the nasal fossae [15]. Maxillary sinuses septation has no uniform shape or number. There is no correlation between the thickness of the Schneiderian membrane and the presence of sinus septation [16].
When disease occurs in the periapical area, inflammatory changes will affect the lining mucosal and ends into maxillary sinusitis [17]. Another pathway for infection spread is either via blood vessels, bone, or lymphatic drainage. Whenever the root apices of necrotic pulp are closed to the maxillary sinus floor, there is a high chance for maxillary sinusitis to occur. This condition is called Odontogenic maxillary sinusitis [17, 18]. Studies showed that dental disease is the most common cause of maxillary sinusitis for patients visiting dental clinics [19].
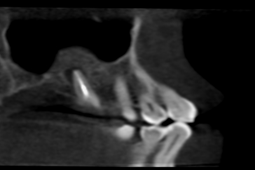
Radicular cyst, which is a cystic lesion caused by necrosis of the pulp, can be enlarged and expands to fulfill the sinus cavity and causes bone destruction of adjacent anatomical structures [20]. See figure 4
 |
 |
|
(A) |
(B) |
Figure 4: 18 years old male patient seeking orthodontic treatment. CBCT show well defined corticated radiolucent oval lesion associated with heavily restored tooth #26. It’s appearance suggesting radicular cyst inside the sinus
Odontogenic maxillary sinusitis is also occurring by complications of improper dental treatment, which influences infection of the sinus cavity. Root canal treatment may cause complications such as over instrumentation, improper obturation, fluid flushing, and intrusion of instruments or biomaterials inside the maxillary cavity [21]. See figure 5

Figure 5: 22 years old male patient came for orthodontic treatment. Tooth #16 went through root canal treatment. Odontogenic sinusitis was noted in the follow up CBCT scan
Prolonged infection results in the oro-antral fistula. Oro-antral communication is also another complication that is incidentally formed during tooth extraction. See Figure 6.
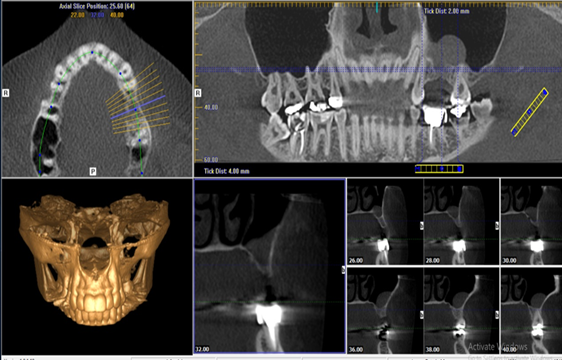
Figure 6: CBCT scan, a panoramic reconstruction, and axial sections show mucosal thickening of the inferior wall of left maxillary sinus at the area of missing the first molar. Discontinuity of the alveolar process is associated with a dome-shaped high-density soft tissue lesion. These findings are suggesting of oro-antral communication/ fistula and maxillary sinusitis.
Improper dental implant treatment could lead to maxillary sinus disease [22-24]. There is no evidence related to gender or age to maxillary sinusitis [25]. See figure 7

Figure 7: 38-year-old male patient imaged for post implant insertion evaluation. Scan showed one of the implants is completely inside the left sinus
Moreover, the thickness of the maxillary alveolar bone is not uniform and ranges between 1-2 mm. Teeth locations have a strong association with infection of maxillary sinuses. A disease initiated in the molars could cause mucosal sinusitis more frequently than if the source of infection was from premolar teeth. Also, there is a correlation between root location and maxillary sinusitis. The palatal root is the most common root that causes maxillary sinusitis. Further, it is followed by the mesiobuccal root for the second molar. To decrease the risk of maxillary sinusitis, it is better to avoid iatrogenic procedure into these roots [26]. See figure 8
 |
 |
|
(A) |
(B) |
Figure 8: 48 years old male patient seeking for denture construction. Odontogenic Lesion was indecently discovered and surgically removed.
Sinusitis can also be of non-odontogenic origin, a soft tissue density mass within the sinuses originating from conditions such as asthma, allergy and polyposis, and in the absence of carious tooth and mucosal thickening not limited to any tooth. Non-odontogenic chronic inflammatory disease of maxillary sinuses associated with a bacterial or fungal infection may cause thickening and sclerosis of the bone. [See figure 9]. Non-odontogenic sinusitis develops as a saprophytic growth in retained secretions in a sinus cavity [7]. Both types of sinusitis can be effectively imaged with CBCT. Its use in imaging diseases of the temporal bone and the inner ear has now been well established.
 |
 |
 |
Figure 9: 66 years female patient came to clinic to restore carious teeth and edentulous spaces. Congenital malformation of the nasal turbinate.
Many of the studies regarding maxillary sinusitis were evaluating the maxillary sinus mucosal thickening. The average mucosal thickness was 6 mm ±3 mm [27]. This finding could reach more than half of patients visiting dental practice [28]. If lining mucosa shows thickness more than 2mm, the chance of presence of lesions such as mucous retention cyst, mucosal polyps, or air-fluid level is appreciated [16]. [See figure 10] Also, it is observed that maxillary sinus mucosa is increased whenever there is an obstruction in the osteo-meatal complex [25].
 |
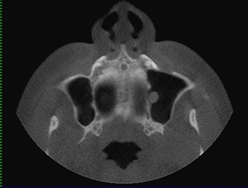 |
Figure 10: 33 years old male patient came to clinic to remove retained root for tooth #17 in maxillary sinus. CBCT was taken five months after surgical removal for follow up. There is polyp located at the medial wall of left maxillary sinus.
Furthermore, one of the most indications that require an understanding of maxillary sinuses is the treatment planning of dental implant in the maxilla, which requires bone grafting and sinus elevation surgery. Augmentation of the maxillary sinus floor is well-documented and considered a conventional treatment method, which allows the rehabilitation of the atrophic posterior maxilla for dental implant osteointegration [10].
CBCT Role in maxillary sinus disease
The panoramic radiograph may play a role in the detection of maxillary sinus disease incidentally with a screening of dental conditions. The discovery of maxillary sinus variation and pathology is made routinely by C.T. scans. Moreover, MRI is better than C.T. scans in the detection of soft tissue structures [7]. Since the CBCT scan machine was invented to be used in dentistry, many dentists become familiar with the interpretation of maxillary abnormalities that affect the quality of prosthesis and the success rate of the dental implant. CBCT is far more successful in identifying dental disease-causing sinusit [8] is. CBCT is useful to determine whether any tooth or any tooth root was more frequently associated with a disease. The multi-planar reconstruction (MPR) in CBCT software helps practitioners for assessment sinus configuration and the presence of roots inside the sinus [29]. The CBCT scan is also indicated to evaluate lesion's healing [30]. Dose levels of CBCT are considerably lower than with medical CT imaging, depending on the selected field of view (FOV). With high-resolution CBCT imaging of the temporal bone, the dose is approximately equivalent to one to two panoramic images. In high-resolution sino-nasal imaging with a large field of view, the dose is approximately equivalent to three panoramic images. At the press of a button, most CBCT scanners can automatically switch between 3D and panoramic imaging modes [31].
The feasibility of CBCT comes from interpreting any anatomic variations as well as lesions, borders, and extensions. Routine examination of the maxillary sinus is required for dental implant planning. Also, it becomes the most requested pre-surgical assessment in dentistry [25]. CBCT can detect pathology in bone more accurately than in soft tissue. It cannot differentiate between soft tissue and fluid attenuation the same way C.T. scans do. It is mainly requested if the disease affected bone tissue. The attenuation limitation of CBCT scans is caused by machine projection geometry, poor contrast resolution, and less sensitivity of scan detector [15].
Upon the use of CBCT scans, Manji et al. classified sinus pathology into one of the five categories: healthy, mucosal thickening > 5mm, polypoidal mucosal thickening, partial opacification, an air-fluid level, and complete opacification [32].
The presence of periodontal pathology was found to be associated with the presence of radio-densities. The presence of diffuse increased attenuation within the sinus cavity should be considered as chronic allergic hypersensitivity or chronic hyperplastic sinusitis and polyposis associated with desiccated and retained mucosal secretions [33].
Differential diagnosis of maxillary sinus disease associated with the presence or absence of dental cause depends on the lesion density (attenuation), extension, location, expansion, the effect on the sinus wall and adjacent structures. CBCT scans diagnose the obstruction of osteo-meatal complex due to pathology or an anatomical variation such as nasal septum deviation. Thickening of maxillary sinus mucosa presents as a radiopaque line or area consistent with mucositis or maxillary sinusitis. The presence of air-fluid levels reveals either trauma or mucus accumulation. The mucous retention cyst is the submucosal accumulation of mucus. It is a dome-shaped well defined soft- tissue density attached to the side of the sinus wall [See figure 11]. Complete opacification of the sinus cavity with the expansion of maxillary walls represents Mucocele. Mucocele may be a destructive lesion, which is caused by inflammation, tumor, or large polyp.
 |
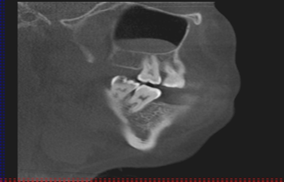 |
Figure 11: Mucous retention cyst
The presence of a benign tumor or cyst will cause expansion of the sinus toward the least resistant anatomical structures, the cavity of the sinus. On the other hand, the malignant lesion will cause massive destruction of the maxillary alveolar bone, teeth, and sinus walls. Infection and malignant lesions inside the sinus cavity mimic the same soft-tissue attenuation while the chronic disease may show sclerosing areas, high-density attenuation surrounding the injury [15, 34]. [See figure 12]
 |
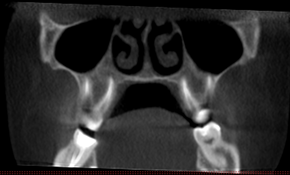 |
Figure 12: Periapical lesion associated with palatal root of tooth #1.6 in 32-year-old female causing sclerotic reaction of bone yet not affecting the corresponding sinus. Sagittal view (LT) and coronal view (RT)
Finally, the diagnosis of maxillary sinus disease is highly appreciated by a CBCT scan. This does not rule the importance of clinical examination and further investigation, such as vitality tests. Anatomical variations of the maxillary sinus are the key to the presence of maxillary sinus disease. Precise diagnosis for reasons of periapical radiolucency before referral to the CBCT scan may identify a poorly recognized anatomical variation, which may cause diagnostic confusion [29].
Conclusions
CBCT examination is the best and convenient imaging tool in the dental practice that can identify the presence of pathology in maxillary sinus before surgery or post-operative complication and follow-up.
Funding: This research received no external funding.
Conflicts of Interest: The authors declare no conflicts of interest.
REFERENCES
- Asaumi R, Sato I, Miwa Y, Imura K, Sunohara M, Kawai T, Yosue T. Understanding the formation of maxillary sinus in Japanese human foetuses using cone beam CT. Surgical and radiologic anatomy. 2010 Oct 1;32(8):745-5
- Safabakhsh M, Moudi E, Khafri S, Abesi F. Radiographic Evaluation of Maxillary Sinus Surgical Risks in Sinus Lifting Surgery Candidates Using Cone Beam Computed Tomography (CBCT). Ann. Dent. Spec. 2019 Apr;7(2):11-8.
- Iranmanesh M, Meybodi EE. Evaluation of The Amount of Artifacts Around Different Implants in Cone Beam Computed Tomography. Ann. Dent. Spec. 2018 Jul 1;6(3):246-9.
- Rafighi A, Sohrabi A, Moslemzadeh SH, Mardani Z. Assessing Pain and Cooperation Levels of Orthodontic Patients Treated with Medium and Heavy Intermaxillary Elastics: a Randomized Clinical Trial. Archives of Pharmacy Practice. 2019 Jan 1;1:19.
- Anatolyevich DD, Vladimirovich KV, Nikolaevna PE, Ivanovna AO, Nikolaevich GA, Viktorovich PS. Microcomputed Tomography in Qualitative and Quantitative Evalua-tion of Dental Enamel Demineralization. Entomology and Applied Science Letters. 2019 Jan 30;5(4):91-102.
- Carmeli G, Artzi Z, Kozlovsky A, Segev Y, Landsberg R. Antral computerized tomography pre‐operative evaluation: relationship between mucosal thickening and maxillary sinus function. Clinical oral implants research. 2011 Jan;22(1):78-82.
- Mafee MF, Tran BH, Chapa AR. Imaging of rhinosinusitis and its complications. Clinical reviews in allergy & immunology. 2006 Jun 1;30(3):165-85.
- Patel NA, Ferguson BJ. Odontogenic sinusitis: an ancient but under-appreciated cause of maxillary sinusitis. Current opinion in otolaryngology & head and neck surgery. 2012 Feb 1;20(1):24-
- Alfaraje, L. Surgical and radiologic anatomy for oral implantology. U.S.: Quintessence, 2013.
- Nkenke E, Stelzle F. Clinical outcomes of sinus floor augmentation for implant placement using autogenous bone or bone substitutes: a systematic review. Clinical oral implants research. 2009 Sep;20:124-33.
- Lu Y, Liu Z, Zhang L, Zhou X, Zheng Q, Duan X, Zheng G, Wang H, Huang D. Associations between maxillary sinus mucosal thickening and apical periodontitis using cone-beam computed tomography scanning: a retrospective study. Journal of endodontics. 2012 Aug 1;38(8):1069-74.
- Jung YH, Nah KS, Cho BH. Maxillary sinus pneumatization after maxillary molar extraction assessed with cone beam computed tomography. Imaging Science in Dentistry. 2009;39(3):109-13.
- Wehrbein H, Diedrich P. Progressive pneumatization of the basal maxillary sinus after extraction and space closure. Fortschritte der Kieferorthopadie. 1992 Apr;53(2):77-83.
- Chan HL, Wang HL. Sinus pathology and anatomy in relation to complications in lateral window sinus augmentation. Implant Dentistry. 2011 Dec 1;20(6):406-12.
- Pharoah, W. A. Oral Radiology principles and interpretation, 6th edition. St. Louis, Missouri: MOSBY ELSEVIER, 2014.
- Sánchez-Pérez A, Boracchia AC, López-Jornet P, Boix-García P. Characterization of the maxillary sinus using cone beam computed tomography. A retrospective radiographic study. Implant dentistry. 2016 Dec 1;25(6):762-9.
- Mehra P, Jeong D. Maxillary sinusitis of odontogenic origin. Current allergy and asthma reports. 2009 May 1;9(3):238-43.
- Mehra P, Murad H. Maxillary sinus disease of odontogenic origin. Otolaryngologic Clinics of North America. 2004 Apr 1;37(2):347-64.
- Maillet M, Bowles WR, McClanahan SL, John MT, Ahmad M. Cone-beam computed tomography evaluation of maxillary sinusitis. Journal of endodontics. 2011 Jun 1;37(6):753-7.
- Riviş M, Văleanu AN. Giant maxillary cyst with intrasinusal evolution. Rom J Morphol Embryol. 2013;54(3):889-92.
- Kawai T, Tanaka R, Yeung AW, von Arx T, Bornstein MM. Frequency and type of incidentally detected radiodensities in the maxillary sinus: a retrospective analysis using cone beam computed tomography (CBCT). Clinical oral investigations. 2019 Mar 8;23(3):1091-9. https://doi.org/10.1007/s00784-018-2541-8.
- Ariji Y, Obayashi N, Goto M, Izumi M, Naitoh M, Kurita K, Shimozato K, Ariji E. Roots of the maxillary first and second molars in horizontal relation to alveolar cortical plates and maxillary sinus: computed tomography assessment for infection spread. Clinical oral investigations. 2006 Mar 1;10(1):35-41.
- Galli SK, Lebowitz RA, Giacchi RJ, Glickman R, Jacobs JB. Chronic sinusitis complicating sinus lift surgery. American Journal of Rhinology. 2001 May;15(3):181-6.
- Watzek G, Bernhart T, Ulm C. Complications of sinus perforations and their management in endodontics. Dental Clinics of North America. 1997 Jul;41(3):563-83.
- Dobele I, Kise L, Apse P, Kragis G, Bigestans A. Radiographic assessment of findings in the maxillary sinus using cone-beam computed tomography. Stomatologija. 2013;15(4):119-22.
- Pagin O, Centurion BS, Rubira-Bullen IR, Capelozza AL. Maxillary sinus and posterior teeth: accessing close relationship by cone-beam computed tomographic scanning in a Brazilian population. Journal of endodontics. 2013 Jun 1;39(6):748-51.
- Deeb R, Malani PN, Gil B, Jafari-Khouzani K, Soltanian-Zadeh H, Patel S, Zacharek MA. Three-dimensional volumetric measurements and analysis of the maxillary sinus. American journal of rhinology & allergy. 2011 May;25(3):152-6.
- Shanbhag S, Karnik P, Shirke P, Shanbhag V. Association between periapical lesions and maxillary sinus mucosal thickening: a retrospective cone-beam computed tomographic study. Journal of endodontics. 2013 Jul 1;39(7):853-7.
- Sekerci AE, Sisman Y, Etoz M, Bulut DG. Aberrant anatomical variation of maxillary sinus mimicking periapical cyst: a report of two cases and role of CBCT in diagnosis. Case reports in dentistry. 2013;2013. DOI: 10.1155/2013/757645. Epub 2013 Apr 24.
- Taschieri S, Del Fabbro M, Corbella S, Weinstein T, Rosano G, Tsesis I. Endoscopic minimally invasive management of a periradicular lesion invading the maxillary sinus. Journal of oral science. 2011;53(4):533-8.
- Miracle AC, Mukherji SK. Conebeam CT of the head and neck, part 2: clinical applications. American Journal of Neuroradiology. 2009 Aug 1;30(7):1285-92.
- Manji A, Faucher J, Resnik RR, Suzuki JB. Prevalence of maxillary sinus pathology in patients considered for sinus augmentation procedures for dental implants. Implant dentistry. 2013 Aug 1;22(4):428-35.
- Kawai T, Tanaka R, Yeung AW, von Arx T, Bornstein MM. Frequency and type of incidentally detected radiodensities in the maxillary sinus: a retrospective analysis using cone beam computed tomography (CBCT). Clinical oral investigations. 2019 Mar 8;23(3):1091-9.
- Koenig et al. Diagnostic Imaging Oral and Maxillofacial. First edition ed. Amirsys: Publishing, INC, 2012.
