Stroke-associated comorbidities in Saudi Arabia
Hussain Gadelkarim Ahmed1,2*, Fahad Khalid Alquwaiay1, Hamoud Fahad AlDhamadi1, Faris Mohammed Suliman alshammari1, Dhari Abdulkarim Saleh Alquwaiay1, Abdulmajeed Mohammed Abdullah Alshammari1, Hamoud Hussain Abdulrahman Alsunitan1
1 College of Medicine, University of Hail, Saudi Arabia
2 Department of Histopathology and Cytology, FMLS, University of Khartoum, Sudan.
Email: hussaingad5 @ gmail.com
ABSTRACT
Background: Stroke is a significant health problem worldwide. There is a limited literature regarding stroke in Saudi Arabia. The aim of this work was to estimate the stroke associated comorbidities in Saudi Arabia. Methodology: In this study, data regarding stroke was collected from the King Khalid Hospital-cardiac Centre, Hail Region, Saudi Arabia. In the present study, about 1187 (92%) of the patients had ischemic stroke and 103 (8%) had hemorrhagic stroke. Hypertension was detected in 43.3% of the patients (39.8% were males and 48.2% were females). Diabetes was identified in 42.8% of the patients (40% were males and 47% were females). Dyslipidemia was noticed in 14.7% of the patients (14.5% were males and 15% were females). Conclusion: There is fluctuation in the incidence rates in stroke in Hail region. The most prevalent stroke type was ischemic type with the men more affected than females. Hypertension, Diabetes, and dyslipidemia were the most comorbid conditions associated with stroke in Hail region.
Key words: stroke, hypertension, diabetes, dyslipidemia, Saudi Arabia, Hail.
INTRODUCTION
Stroke is a leading cause of death and disability, especially in low-income and middle-income countries [1]. In the past decades, the rate of stroke is considered to be noticeably higher in high income countries compared with low- and middle-income nations. In the upcoming years, the rate of stroke was expected to decrease in the high income countries and may be doubled up in regions such as rural South Africa and South India. Moreover, stroke-related disability and mortality rate may grow up to 10 times greater in nations with unwarranted medical cared compared with people in developed world. The most apparent causes of this difference include, the insufficiency of primary care treatment to screen patients for the risk of stroke, as well as, lowering of stroke rated risk factors [2]. There are many modifiable risk factors for the prevention of stroke including active cigarette smoking, sustained high blood, type 2 diabetes mellitus, obesity, lack of physical activity, poor diet, too much alcohol usage, atrial fibrillation, abnormal lipid profile, socioeconomic status, and psychosocial stress/depression [3-5]. It was reported that some of antihypertensive drugs may elevate the erraticism of blood pressure and eventually elevate stroke risk. A recent study has proposed the use of antiplatelet drug (unless an indication for anticoagulation exists) as a suitable prevention drug [6].
Due to time stress in ischemic stroke treatment by the thrombolytic drugs, there is an increasing rate of misdiagnosis. Within the constricted time window of thrombolysis, a false-positive stroke diagnosis can lead to defective and possibly risky thrombolysis. The terms "Stroke Mimic" (SM = false-positive stroke diagnosis) and "Stroke Chameleon" (SC = false-negative stroke diagnosis) were suggested for misdiagnosis in this field [7].
Stroke incidence and death are growing in the Middle-East and North African (MENA) states. MENA patients who are relatively younger are considered as having increased diabetic prevalence with relatively greater severity of ischemic stroke, usually of atherosclerotic or microvascular type [8]. Recent data regarding the first-stroke incidence in Saudi Arabia, in general, are infrequent and even highly deficient. Considering the forthcoming aging of Saudi population due to advancement in overall health care including primary health care and other medical services, an increased number of at risk population is expected. Dramatic increase in the stroke-related comorbidities may be a further factor leading to an escalating figure of stroke [9]. Therefore, the objective of the present study was to assess the stroke-associated comorbidities in Saudi Arabia.
MATERIALS AND METHODS
In this study, data regarding stroke was obtained from the King Khalid Hospital-cardiac Centre, Hail Region, Saudi Arabia. Data referring to patients with stroke who were diagnosed during the period from 2010 to 2016 were included.
Data regarding the underlying risk factors such as hypertension, diabetes, dyslipidemia, and demographical characteristics, and outcome were also reviewed.
Statistical analysis:
Data analysis was done by using the Statistical Package for Social Sciences (SPSS version 16; SPSS Inc, Chicago, IL). The 95% confidence level was considered.
Ethical consent:
Our study protocol was confirmed according to the 2013 Declaration of Helsinki and this study was approved by the ethics committee of the College of Medicine, University of Hail, Saudi Arabia.
RESULTS
The study reviewed the records related to 1290 patients with stroke aged 20 to 100 years with a mean age of 68 years’ old that 761(59%) were males and 529(41%) were females. About 1187(92%) of the patients were attended with ischemic stroke and the remaining 103(8%) with hemorrhagic stroke, as shown in Fig 1.
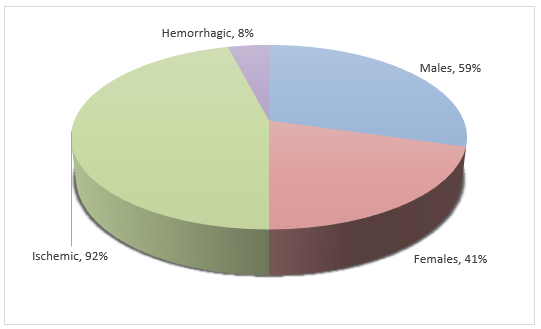
Figure 1. Description of the patients by sex and stroke type
Out of the 1290 patients, 1115/1290(86.4%) were Saudi civilian and 175/1290(13.6%) were non-Saudi persons. With regards to the age, the great majority of patients were found at the age group 66-75 years followed by 76-85, and 56-65 years representing 322, 297, and 207 patients, respectively, as indicated in Table 1, and Fig 2. With regards to the year of admission, the highest frequency of admission was in the year 2011 followed by 2014, and 2010 constituting 257, 250, and 224, correspondingly, as indicated in Table 1, and Fig 3.
Table 1. Description of the study subjects by demographical characteristics and year of admission
|
Variable |
Males |
Females |
Total |
|
Nationality |
|
|
|
|
Saudi |
604 |
511 |
1115 |
|
Non-Saudi |
157 |
18 |
175 |
|
Total |
761 |
529 |
1290 |
|
Age group |
|
|
|
|
<45 years |
91 |
29 |
120 |
|
46-55 |
98 |
49 |
147 |
|
56-65 |
121 |
86 |
207 |
|
66-75 |
181 |
141 |
322 |
|
76-85 |
158 |
139 |
297 |
|
86+ |
112 |
85 |
197 |
|
Total |
761 |
529 |
1290 |
|
Year of admission |
|
|
|
|
2010 |
117 |
107 |
224 |
|
2011 |
156 |
101 |
257 |
|
2012 |
96 |
58 |
154 |
|
2013 |
61 |
37 |
98 |
|
2014 |
143 |
107 |
250 |
|
2015 |
125 |
86 |
211 |
|
2016 |
63 |
33 |
96 |
|
Total |
761 |
529 |
1290 |
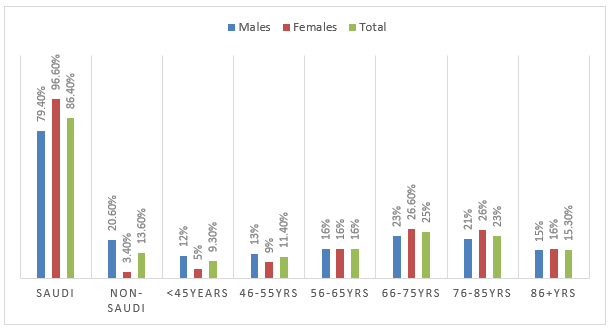
Figure 2. Description of the patients by nationality and age
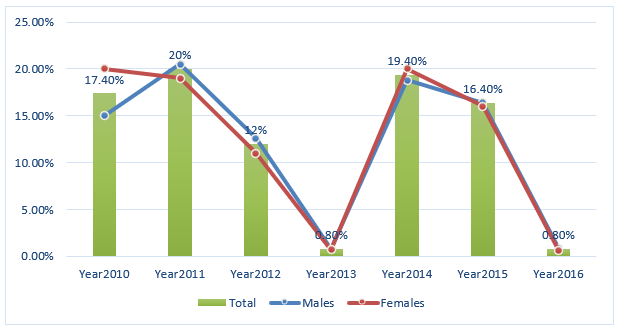
Figure 3. Description of the patients by the year of admission
Hypertension was detected in 558/1290(43.3%) of the patients that 303/761(39.8%) were males and 255/529(48.2%) were females.
Diabetes was identified in 552/1290(42.8%) of the patients that 304/761(40%) were males and 248/529(47%) were females.
Dyslipidemia was noticed in 189/1290(14.7%) of the patients that 110/761(14.5%) were males and 79/529(15%) were females.
Congestive Heart Disease (CHD) was noticed in 137/1290(10.6%) of the patients that 86/761(11.3%) were males and 51/529(9.6%) were females.
Fort the outcomes, the majority of patients were normally discharged which account for 757/1290(58.7%). However, 312/1290(24%) of the patients died that (186/761(24.4%) were males and 126/529(23.8%) were females, as indicated in Table 2 and Fig 5.
DAMA was regarded in 191/1290 (14.8%) that 145/761(19%) were males and 46/529(8.7%) were females, as indicated in Table 2 and Fig 5.
Table 2. Description of the study subjects by sex and comorbidities
|
Variable |
Males |
Females |
Total |
P-value |
|
Hypertension |
|
|
|
0.003 |
|
Yes |
303 |
255 |
558 |
|
|
No |
458 |
274 |
732 |
|
|
Total |
761 |
529 |
1290 |
|
|
Diabetes |
|
|
|
0.013 |
|
Yes |
304 |
248 |
552 |
|
|
No |
457 |
281 |
738 |
|
|
Total |
761 |
529 |
1290 |
|
|
Dyslipidemia |
|
|
|
0.811 |
|
Yes |
110 |
79 |
189 |
|
|
No |
651 |
450 |
1101 |
|
|
Total |
761 |
529 |
1290 |
|
|
CHD |
|
|
|
0.342 |
|
Yes |
86 |
51 |
137 |
|
|
No |
675 |
478 |
1153 |
|
|
Total |
761 |
529 |
1290 |
|
|
Outcomes |
|
|
|
|
|
Discharged |
410 |
347 |
757 |
|
|
Died |
186 |
126 |
312 |
|
|
DAMA |
145 |
46 |
191 |
|
|
Transferred |
20 |
10 |
30 |
|
|
Total |
761 |
529 |
1290 |
|
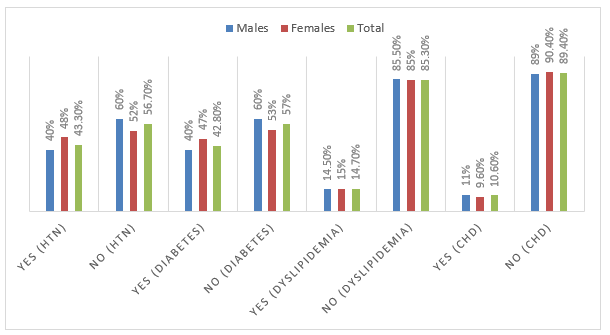
Figure 4. Description of the patients by comorbidities
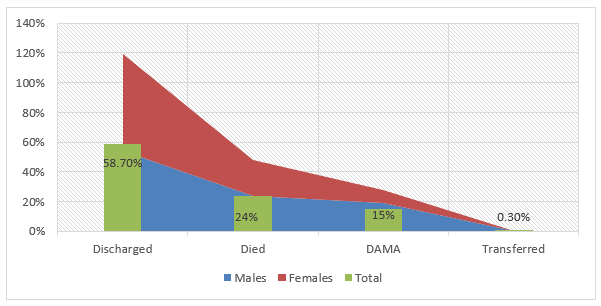
Figure 5. Description of the patients by outcomes
DISCUSSION
In the present studies, a series of patients in several years have been retrospectively reviewed. The incidence rates have fluctuated with the highest increase in the year 2011 and the lowest in the year 2013 and the year 2013. With the lack of literature in this regard, there is no specific explanation for these incidence rates fluctuation. The findings of the present study show relatively increased incidence amongst the younger population. It was found that there were tendencies in the direction of growing stroke incidence at younger ages, which represents great public health significance because strokes in younger patients carry the potential for bigger lifetime burden of disability because some potential contributors recognized for this tendency are modifiable [10]. It was suggested that, the burden of the stroke may carry on escalating in a long time if not the risk factors in low-income nations are efficiently controlled [11].
The findings of the present study showed that stroke was more common among males compared to females. Such findings were previously reported in some studies [12,13]. Worldwide, though women have severe sort of the disease, stroke is frequently encountered among men [12]. The sex-related difference was partly explained by several customary cardiovascular risk factors [13].
The majority of cases of stroke in the current study were identified with ischemic stroke type and lower number of cases were found with hemorrhagic types. Major pathological stroke types (ischemic stroke [IS], primary intracerebral hemorrhage [ICH], and subarachnoid hemorrhage) and IS subtypes, have different risk factors, management, and prognosis [14].
Ischemic stroke is an upsetting brain injury causing a great death and considerable loss of function. Age and sex possess a multifaceted and shared influence on ischemic stroke risk and pathophysiology. Aging is the most powerful non-changeable risk factor for ischemic stroke. Aged stroke patients are considered as having greater mortality and morbidity and worse functional retrieval compared with young equivalents. During the younger ages, the prevalence of stroke is higher among men; whereas, with increasing of age, elder women are more susceptible [15].
However, a decrease of change in IS and ICH incidence may reflect a trend toward increased incidence of younger strokes [14].
In the current study, hypertension was detected in 43.3% of the patients (39.8% were males and 48.2% were females). The strong relationship between stroke and hypertension has been the finding of a number of studies and trials [16]. Hypertension is the distinct utmost significant amendable risk factor for adult stroke. Stroke mortality has significantly declined over the last 5 decades; this decline has been mainly associated with improved blood pressure control [17, 18].
Diabetes was identified in 42.8% of the patients (40% were males and 47% were females). Patients with diabetes have almost double the risk of stroke compared to nondiabetics [19]. Diabetes leads to different microvascular and macrovascular alterations regularly terminating in major clinical complications, one of which is stroke. This augmented risk is often perceived in persons with diabetes and is attending with worse clinical consequences (with greater rate of death), particularly after ischemic stroke [20].
Dyslipidemia was noticed in 14.7% of the patients (14.5% were males and 15% were females). High triglyceride (TG) levels and low HDL cholesterol (HDL-C) levels are risk factors for cardiovascular disease [21]. In a disease-free population, low-density lipoprotein cholesterol LDL-C and non-HDL-C baseline measures are suggestively accompanying the risk of ischemic stroke [22]. Dyslipidemia and hypertriglyceridemia may be more prevalent in children with arterial ischemic stroke compared with stroke-free children [23].
Congestive Heart Disease (CHD) was noticed in 10.6% of the patients (11.3% were males and 9.6%) were females). Heart failure has been linked to an amplified risk for ischemic stroke [24]. For a single patient with both atrial fibrillation and heart failure, stroke risk is one of the most noticeable modifying factors for later morbidity and mortality [25].
In the present study, more than 58% of the patients were discharged normally, but about 24.4% of the patients died. This percentage is relatively higher, which may be attributed to several factors including management and some demographical or comorbidities factors, which might not be available in the present study.
CONCLUSION
There is fluctuation in the incidence rates in stroke in Hail region. Ischemic stroke is the most prevalent stroke type with the males more affected than females. Hypertension, diabetes, and dyslipidemia were the most comorbid conditions associated with stroke in the Hail region. With the lack of literature about stroke from Saudi Arabia, future studies are highly recommended.
ACKNOWLEDGMENT
The authors would like to thank the people in King Khalid Hospital for their help support in data collection.
REFERENCES
- O'Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, Rao-Melacini P, Zhang X, Pais P, Agapay S, Lopez-Jaramillo P. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. The lancet. 2016 Aug 20;388(10046):761-75. doi: 10.1016/S0140-6736(16)30506-2.
- Norrving B, Kissela B. The global burden of stroke and need for a continuum of care. Neurology. 2013 Jan 15;80(3 Supplement 2):S5-1 doi: 10.1212/WNL.0b013e3182762397.
- Kuklina EV, Tong X, George MG, Bansil P. Epidemiology and prevention of stroke: a worldwide perspective. Expert review of neurotherapeutics. 2012 Feb 1;12(2):199-208. doi:10.1586/ern.11.99
- Nakibuuka J, Sajatovic M, Nankabirwa J, Furlan AJ, Kayima J, Ddumba E, Katabira E, Byakika-Tusiime J. Stroke-risk factors differ between rural and urban communities: population survey in Central Uganda. Neuroepidemiology. 2015;44(3):156-65. doi:10.1159/000381453.
- Namale G, Kamacooko O, Kinengyere A, Yperzeele L, Cras P, Ddumba E, Seeley J, Newton R. Risk factors for hemorrhagic and ischemic stroke in sub-Saharan Africa. Journal of tropical medicine. 2018;2018. doi:10.1155/2018/4650851.
- Guzik A, Bushnell C. Stroke epidemiology and risk factor management. CONTINUUM: Lifelong Learning in Neurology. 2017 Feb 1;23(1):15-39. doi: 10.1212/CON.000000000000041
- Erbguth F. Stroke Mimics und Stroke Chamäleons–Differenzialdiagnose des Schlaganfalls. Fortschritte der Neurologie· Psychiatrie. 2017 Dec;85(12):747-64. doi: 10.1055/s-0043-111889.
- Rukn SA, Mazya MV, Hentati F, Sassi SB, Nabli F, Said Z, Faouzi B, Hashim H, Abd-Allah F, Mansouri B, Kesraoui S. Stroke in the Middle-East and North Africa: A 2-year prospective observational study of stroke characteristics in the region—Results from the Safe Implementation of Treatments in Stroke (SITS)–Middle-East and North African (MENA). International Journal of Stroke. 2019 Oct;14(7):715-22. doi: 10.1177/1747493019830331.
- Alhazzani AA, Mahfouz AA, Abolyazid AY, Awadalla NJ, Aftab R, Faraheen A, Khalil SN. Study of stroke incidence in the aseer region, Southwestern Saudi Arabia. International journal of environmental research and public health. 2018 Feb;15(2):215. doi:10.3390/ijerph15020215.
- Kissela BM, Khoury JC, Alwell K, Moomaw CJ, Woo D, Adeoye O, Flaherty ML, Khatri P, Ferioli S, La Rosa FD, Broderick JP. Age at stroke: temporal trends in stroke incidence in a large, biracial population. Neurology. 2012 Oct 23;79(17):1781-7. doi:1212/WNL.0b013e318270401d.
- Wang J, Bai L, Shi M, Yang L, An Z, Li B, Zhao W, Gu H, Zhan C, Tu J, Ning X. Trends in age of first-ever stroke following increased incidence and life expectancy in a low-income chinese population. Stroke. 2016 Apr;47(4):929-35. doi: 10.1161/STROKEAHA.115.012466.
- Appelros P, Stegmayr B, Terént A. Sex differences in stroke epidemiology: a systematic review. Stroke. 2009 Apr 1;40(4):1082-90. doi: 10.1161/STROKEAHA.108.540781.
- Wang Y, Dai Y, Zheng J, Xie Y, Guo R, Guo X, Sun G, Sun Z, Sun Y, Zheng L. Sex difference in the incidence of stroke and its corresponding influence factors: results from a follow-up 8.4 years of rural China hypertensive prospective cohort study. Lipids in health and disease. 2019 Dec 1;18(1):72. doi:10.1186/s12944-019-1010-y.
- Krishnamurthi RV, Barker-Collo S, Parag V, Parmar P, Witt E, Jones A, Mahon S, Anderson CS, Barber PA, Feigin VL. Stroke incidence by major pathological type and ischemic subtypes in the Auckland regional community stroke studies: changes between 2002 and 2011. Stroke. 2018 Jan;49(1):3-10. doi: 10.1161/STROKEAHA.117.019358.
- Roy-O’Reilly M, McCullough LD. Age and sex are critical factors in ischemic stroke pathology. Endocrinology. 2018 Aug;159(8):3120-31. doi: 10.1210/en.2018-00465.
- Pistoia F, Sacco S, Degan D, Tiseo C, Ornello R, Carolei A. Hypertension and stroke: epidemiological aspects and clinical evaluation. High Blood Pressure & Cardiovascular Prevention. 2016 Mar 1;23(1):9-18. doi: 10.1007/s40292-015-0115-2.
- Kupferman JC, Zafeiriou DI, Lande MB, Kirkham FJ, Pavlakis SG. Stroke and hypertension in children and adolescents. Journal of child neurology. 2017 Mar;32(4):408- doi: 10.1177/0883073816685240.
- Pathak A, Kumar P, Pandit AK, Chakravarty K, Misra S, Yadav AK, Prasad K. Is Prevalence of Hypertension Increasing in First-Ever Stroke Patients?: A Hospital-Based Cross-Sectional Study. Annals of neurosciences. 2018;25(4):219-22. doi:10.1159/000487066
- Hill MD. Stroke and diabetes mellitus. Handb Clin Neurol. 2014;126:167-74. doi: 10.1016/B978-0-444-53480-4.00012-6.
- Chen R, Ovbiagele B, Feng W. Diabetes and stroke: epidemiology, pathophysiology, pharmaceuticals and outcomes. The American journal of the medical sciences. 2016 Apr 1;351(4):380-6. doi:10.1016/j.amjms.2016.01.011.
- Lee JS, Chang PY, Zhang Y, Kizer JR, Best LG, Howard BV. Triglyceride and HDL-C dyslipidemia and risks of coronary heart disease and ischemic stroke by glycemic dysregulation status: the strong heart study. Diabetes care. 2017 Apr 1;40(4):529-37. doi:10.2337/dc16-1958.
- Glasser SP, Mosher A, Howard G, Banach M. What is the association of lipid levels and incident stroke?. International journal of cardiology. 2016 Oct 1;220:890-4. doi:10.1016/j.ijcard.2016.06.091
- Sultan S, Dowling M, Kirton A, DeVeber G, Linds A, Elkind MS, Bernard T, Hernandez M, Rivkin M, Kopyta I, Ichord R. Dyslipidemia in children with arterial ischemic stroke: prevalence and risk factors. Pediatric neurology. 2018 Jan 1;78:46-54. doi:10.1016/j.pediatrneurol.2017.09.019
- Kang SH, Kim J, Park JJ, Oh IY, Yoon CH, Kim HJ, Kim K, Choi DJ. Risk of stroke in congestive heart failure with and without atrial fibrillation. International journal of cardiology. 2017 Dec 1;248:182-7. doi: 10.1016/j.ijcard.2017.07.056.
- Abraham JM, Connolly SJ. Atrial fibrillation in heart failure: stroke risk stratification and anticoagulation. Heart failure reviews. 2014 May 1;19(3):305-13. doi: 10.1007/s10741-014-9420-4.
