Evaluation of the Effectiveness of Cost-free Nutrition Programme on Children in Reo Health District, Burkina Faso
Compaore Wendinpuikondo Raketa Ella1*, Ouedraogo Ousmane1, Souho Tiatou2, Nikiema Philippe Augustin1, Virginio Pietra3, Ellahi Basma4, Amouzou Sabiba Kou’santa Emile2, Meda Nicolas5, Dicko Hama Mamoudou1
1Department of Biochemistry and Microbiology, University Joseph KI-ZERBO, Ouagadougou, Burkina Faso
2Faculty of Sciences and Techniques, University of Kara, Kara, Togo
3Medicus Mundi Italy, Koudougou, Burkina Faso
4Faculty of Health and Social Care, University of Chester, Chester, United Kingdom
5Department of Public Health, University Joseph KI-ZERBO, Ouagadougou, Burkina Faso.
*Email: rakibf @ gmail.com
ABSTRACT
Background: The community management for acute malnutrition (CMAM) was started in 2012 with the aim to impact the lives of a large number of children suffering from acute malnutrition without any cost. Objective: The study aimed at evaluating the effectiveness of the CMAM program on severe acute malnutrition (SAM) and moderate acute malnutrition (MAM) treatment. Methods: Children aged 6 to 59 months were screened for malnutrition in a complementary compulsory screening program. Acutely malnourished children underwent free medical and nutritional treatment. Evaluation of the CMAM program implementation was performed by comparison with paid services by collecting data from malnourished children’s parents. Results: From the 64458 screened children, 835 were diagnosed as new acutely malnourished cases and referred to health centers for treatment. The anthropometric parameters (MUAC, weight, height) have significantly improved from the time of admission to the end of treatment. Performance indicators using the Sphere standards were above the expected level for outpatient treatment but for inpatient treatment, it failed to meet the expected standard. Poverty and the use of traditional medicine to treat malnutrition, distance, availability, and cost of transportation to the health center were significant barriers to the continuation of healthcare services. Conclusion: The CMAM program is effective. It covered and allowed the treatment of several children presenting the number of pathologies reducing children's morbidity and mortality. In order to increase children’s nutritional status, it will be helpful to work with traditional healers.
Key words: acute malnutrition, effectiveness, screening, malnourished children, ready to use therapeutic foods, ready to use supplementary foods.
INTRODUCTION
According to the World Health Organization (WHO), malnutrition is characterized by a pathological condition resulting from deficiency, excess or imbalance of one or more nutrients [1]. This may manifest itself clinically or be detectable by biochemical, anthropometric and physiological analyses [1]. Malnutrition is the underlying cause of 3.5 million deaths of children under the age of five every year [2]. Most of these children live in South Asia and sub-Saharan Africa [2]. The United Nation’s agreed sustainable development goals (SDG) have presented a unique opportunity to focus on nutritional interventions and their importance as a factor of development [3]. It is becoming ever clearer that several components of the SDGs would not be achieved without reduction of malnutrition [4].
Until recently, the treatment of severe acute malnutrition (SAM) was under hospital care, which greatly limited its coverage and impact [5]. Also, in 2001, therapeutic support to a community-based approach was developed to treat acute malnutrition [6]. The approach aimed to reach the maximum number of children suffering from acute malnutrition and ensure access and coverage by providing treatment in as many decentralized sites as possible instead of a few health facilities located in urban centers. Burkina Faso is one of the poorest sub-Saharan countries in Africa, where the prevalence of acute malnutrition is around 10% [7, 8] support is undertaken according to the protocol of the Ministry of Health (MOH) as a part of a transition to scaling up its community-based management [9]. The community-based approach is used to detect, in a timely manner, cases of severe acute malnutrition in the community and provide a treatment administered at home or in health centers to prevent the death of children [10].
The overall objective of this study was to evaluate the CMAM program on SAM and moderate acute malnutrition (MAM) and assess whether a cost-free program resulted in the ineffectiveness of treatment.
METHODS
The health district of Reo is located in the Midwest of Burkina Faso, around 115 km from Ouagadougou the capital and 15 km from Koudougou, the capital of the region. Its area is 5165 km² and is inhabited by 351081 people [11]. In 2012, the CMAM program was implemented in Reo district comprising of 174 villages.
During 2013, healthcare providers of 45 health wide scale in the district were trained on ambulatory management of acute malnutrition (AM). Periodic (every three months) household screening campaigns were performed to assess malnutrition. All children aged 6-59 months were measured and screened for eligibility for treatment in each village of the district. The 450 community health workers (CHW) of the district carried out measurements of mid-upper arm circumference (MUAC) using WHO standard criteria: SAM criteria (MUAC < 115 mm) and/or bilateral pitting edema of the nutritional origin or MAM criteria (115 mm ≤ MUAC < 125 mm) [3]. Children, whose anthropometric parameters follow WHO standard criteria [3], were eligible to be included.
Inclusion criteria:
Children aged 6-59 months, and diagnosed as malnourished and not receiving treatment.
Exclusion criteria:
Malnourished children below 6 months or above 5 years of age, and/or malnourished children under treatment.
Newly identified AM children were recruited into the CMAM program following informed consent obtained from their mother. The participants were exposed to treatment as an inpatient or outpatient according to WHO criteria as above [3]. The duration of inpatient treatment was generally short (following the 3 phases guidance from WHO [3]), lasting between 3 and 7 days; after treatment, the patient was referred to the health center for continued outpatient care. Data to evaluate the effectiveness of the treatment was collected in all the district health centers.
In close collaboration with the Ministry of Health (MOH) system, UNICEF staff ensured the delivery of nutritional inputs at the district level. The World Food Programme (WFP) supplied products for moderate malnutrition such as corn soya blend (CSB), vegetable oil and supplementary food directly to health centers.
Following verbal consent, data were collected from the children’s mother or caregiver using a structured, validated questionnaire completed by the community health workers. Additional data was compiled through the patient’s registry and treatment records and examination results of the acute malnourished (AM) children.
Data collected included socio-demographic variables (residence and gender); and anthropometric variables (weight, height/length, MUAC, and age). Clinical variables (associated infections, presence or absence of edema) and other clinical blood variables (hemoglobin rate, malaria test, and blood glucose levels) data were collected, although not all are reported in this article. Pelletier, suggests MUAC is an important indicator to use (early or late) nutritional and/or medical care and defines the risk of mortality [12]. MUAC, a simple paper armband measure was used practically, accurately and visually to identify malnutrition in children in any setting [12].
Drabkin colorimetric method was used for determination of hemoglobin levels [13]. The SD (standard diagnosis) BIOLINE Malaria Antigen p.f/p.v test was used for detection of malaria [14]. The automated method was used to determine blood glucose levels [15].
The weight for height Z score, the age for MUAC and the presence of edema were calculated to define acute malnutrition. The median of the MUAC was calculated. Indicators such as duration of stay, average weight gain, cured rate[1], death rate[2] and default rate[3] from the program were assessed according to CMAM methodology [16].
The quality of acute malnutrition screening was assessed by the MUAC median of confirmed SAM cases at the health centers according to Pelletier. MUAC admission analysis provides useful information on the precocity of the recruitment of the case.
Data were verified by the researchers, then entered into using the Statistical Package for the Social Sciences (SPSS, IBM statistics version 20) and analyzed accordingly. The differences between the groups (age and gender) were assessed and statistical significance was set at p < 0.05 with a 95% confidence interval. The indicators outlined above were considered for data interpretation.
The results from the evaluation of the change in malnutrition status and the cost-free impact of the intervention are presented.
RESULTS
Screening of children aged 6-59 was undertaken using 450 trained community health workers (4-7 July, 2013). This resulted in the measurement of a total of 64468 children, the population of children in the area. Of this population, eight hundred and thirty-five (835) newly diagnosed AM children, aged 6-59 months, were identified, with or without medical complications through screening. Among them, 373 were SAM new cases and 462 were MAM new cases. These new cases were referred for treatment at the health centers.
Figure 1 reports the responses of parents/caregivers in Reo district to the primary source of care accessed when a child is sick. The majority reported the use of traditional medicine as a first step in the treatment of malnutrition at home, rather than seeking health ministry medical services. Our findings suggest the need for community health workers to actively identify such cases as a part of their activity in the community.
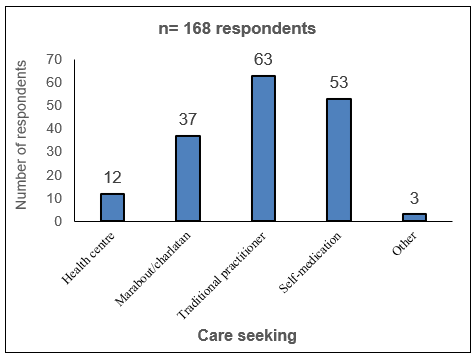
Figure 1: The primary sources of healthcare for parents of ill children in Reo district
Among the cases referred to complications to the hospital (n=8), there were 87.5% (n=7) with bilateral edema (Table 1). The biological examinations revealed that 50% (n=4) of the malnourished children in the hospital suffered from moderate anemia, 25% (n=2) with severe anemia, 25% (n=2) with moderate hypoglycemia and 87.5% (n=7) with malaria, diarrhea and vomiting (Table 1).
Table 1: The complications observed in SAM patients
|
Complications |
n= 8 (number of cases) |
||||
|
Oedema |
Degree |
0 |
+ |
++ |
+++ |
|
|
Number (%) |
1 (12.5) |
0 (0 ) |
2 (25) |
5 (62.5) |
|
Anemia |
Degree |
None |
Moderate |
Severe |
|
|
|
Number (%) |
2 (25) |
4 (50) |
2 (25) |
|
|
Malaria, fever, diarrhea |
Diagnostic |
RDT- |
RDT + |
|
|
|
|
Number (%) |
1 (12.5) |
7 (87.5) |
|
|
|
Hypoglycemia |
Degree |
None |
Moderate |
Severe |
|
|
|
Number (%) |
6 (75) |
2 (25) |
0 (0) |
|
+: edema at the feed only ++: edema at the hand and feed +++: generalized edema
The hospitalized cases that had some complications were treated as recommended by the WHO protocol [17]. Two cases of SAM children were referred outside the health district to intensive nutritional support due to the severity of the malnutrition and complications; and these were excluded from the data presented.
Table 2 shows the distribution of malnourished children by age and gender attending health centers. It indicates that the proportion of children aged 6-23 months and 24-59 months were 75.6% and 24.4% respectively and there is a significant difference between the age groups affected by acute malnutrition (p< 0.05) where the most affected was the 6-23 months age group.
Table 2: Distribution of malnourished children (n) by age and gender attending medical centers in Reo health district
|
SAM n |
MAM n |
Total n (%) |
p |
||
|
Gender |
Male |
180 |
176 |
356 (43) |
0,42 |
|
Female |
193 |
286 |
479 (57) |
||
|
Total |
373 |
462 |
835 (100) |
||
|
Male n |
Female n |
Total n (%) |
p |
||
|
Type of AM |
SAM |
180 |
193 |
373 (45) |
0,52 |
|
MAM |
176 |
286 |
462 (55) |
||
|
Total |
356 |
479 |
835 (100) |
||
|
Male n |
Female n |
Total n (%) |
p |
||
|
Age group (months) |
6-23 |
268 |
363 |
631 (76) |
0,04 |
|
24-59 |
88 |
116 |
204 (24) |
||
|
Total |
356 |
479 |
835 (100) |
Table 3 shows the anthropometric parameters of out-patients and in-patients on admission to the hospital and the cure profile (discharge data). This enables assessment of the variation of treatment. The MUAC median of the SAM was 110 mm. The risk of mortality was high on the assessment of children for many SAM patients (in and outpatients) since they had MUAC values less than the recommended value [3]. The data indicates there is an improvement in all nutrition indicators i.e. height, weight and MUAC.
Table 3: The anthropometric parameters of the patients (n= 370) on admission and cured
|
Type of AM |
Measure |
Height (cm) admission |
Height (cm) cured |
MUAC (mm) admission |
MUAC (mm) cured |
Weight (kg) admission |
Weight (kg) cured |
|
MAM |
Median |
72 |
74 |
120 |
127 |
7.4 |
8.0 |
|
|
Mini* |
57 |
59 |
115 |
120 |
4.5 |
5.7 |
|
|
Max* |
100 |
100 |
130 |
180 |
13.0 |
13.7 |
|
SAM ambulatory |
Median |
72 |
74 |
110 |
124 |
6.5 |
7.8 |
|
|
Mini* |
55 |
62 |
80 |
115 |
3.5 |
5.0 |
|
|
Max* |
120 |
120 |
130 |
150 |
12.0 |
66.0 |
|
SAM Hospital |
Median |
77 |
80 |
112 |
117 |
8.0 |
8.2 |
|
|
Mini* |
57 |
57 |
105 |
105 |
3.6 |
3.6 |
|
|
Max* |
87 |
87 |
126 |
126 |
8.6 |
9.5 |
*Max: Maximum, Mini: Minimum
Figure 2 shows the duration of treatment for SAM children. Cure average was 10 weeks (mini 3; max 19). There were 14 cases of SAM children who abandoned treatment between 7 to 14 weeks of treatment and 7 cases between 1 to 4 weeks of treatment. The average weight gain for the cured inpatients (n = 6) was 7.54±1g/kg/day (data not shown). Figure 3 shows the duration of stay for MAM patients. Cure average was 12 weeks [min 4; max 18].
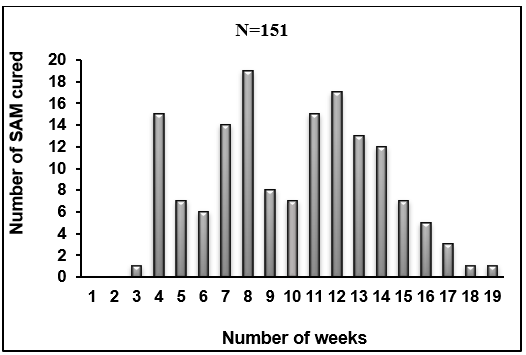
Figure 2: Duration of stay for SAM children (until cured)

Figure 3: Duration of stay for the MAM children (until cured)
Table 4 shows the performance indicators in relation to the treatment of MAM and SAM patients.
For MAM and SAM (ambulatory) outpatients, the average rate was high (89 and 87%, respectively).
Table 4: Performance indicators for the outpatients and inpatients treated
|
Type of AM |
Cure rate |
Death rate |
Default rate |
Total |
|
|
n (%) |
n (%) |
|
n (%) |
|
MAM |
170 (89) |
1 (1) |
19 (10) |
190 (100) |
|
SAM ambulatory |
151 (87) |
2 (1) |
21 (12) |
174 (100) |
|
SAM hospital |
4 (67) |
2 (33) |
0 (0) |
6 (100) |
Table 5 shows performance indicators for inpatients and outpatients by gender. The recovery rates for male and female children are similar in both MAM and SAM (ambulatory); however, the recovery rate for males is much less than for females for the SAM hospitalized patients. However, from the small numbers admitted, it is difficult to state if this difference is significant.
Table 5: Performance indicators for the outpatients and inpatients treated by gender
|
Type of AM |
Gender |
Cure rate n (%) |
Death rate n (%) |
Default rate n (%) |
Total n (%) |
|
MAM |
M |
61 (32.1) |
1 (0.5) |
6 (3.2) |
68 (35.8) |
|
|
F |
109 (57.4) |
0 (0.0) |
13 (6.8) |
122 (64.2) |
|
SAM ambulatory |
M |
67 (38.5) |
1 (0.6) |
7 (4.0) |
75 (43.1) |
|
|
F |
84 (48.3) |
1 (0.6) |
14 (8.0) |
99 (56.9) |
|
SAM hospital |
M |
1 (17.0) |
2 (33.0) |
0 (0.0) |
3 (50.0) |
|
|
F |
3 (50.0) |
0 (0.0) |
0 (0.0) |
3 (50.0) |
DISCUSSION
The CMAM standards recommend 5% to 20% of SAM cases are referred to as inpatients. In all SAM patients, 80% must be outpatients and less than 20% inpatients [18]. In our study, we observed that there were fewer admissions of SAM inpatients (2%, n=8) compared to all of SAM patients treated (n=373). This difference can in part be explained by the period of screening, which was undertaken in the summer when the availability of foods is better and the nourishment is potentially better.
Children aged 6-23 months age group had a higher prevalence of AM compared to age 24-59 months. This finding confirms what was established elsewhere in Burkina Faso [19, 20]. Supplementary feeding practices were observed as not being adequate during the early growth period [21-23]. Late introduction of foods, low consumption and the nutritional quality of these foods (ie those that have low energy density and poorly balanced in macro and micronutrients) are the factors which are recognized as leading to malnutrition. In Burkina Faso, only 11.4% of children aged 6 to 23 months were reported to receive the minimally acceptable food intakes [23]. Furthermore, it was reported that in African countries the first supplementary foods, in addition to breast milk, were produced at the household level and did not cover the nutritional needs of young children [24].
The mean duration of SAM stay was 10 weeks but this is higher than the Sphere standards of 8 weeks, suggesting a low efficiency of the treatment. However, this average is lower than that recorded in 2014 which was 11 weeks [19]. The long duration of treatment was commonly related to late admissions or faltering during treatment, inconsistency in supplies, or abscondment and sometimes despite training efforts at the start of the program, the lack of adherence to the MOH protocol by some health workers was observed resulting in longer treatment or cessation of treatment.
In some cases, children recovered quicker and earlier than the Sphere standard of 8 weeks. However, as the recommendation is 8 weeks, the child is kept in the program until the discharge period set.
The mean duration of recovery for MAM was 12 weeks, suggesting the low efficiency of treatment. Monitoring of the MAM every two weeks not only could explain the long duration but also contributed to the default of treatment or complications if the RUSF (plumpy/sup®) is not given at home. The cases that had a duration of treatment of more than 16 weeks were deemed to not respond to treatment and were referred accordingly.
The various causes of failure of treatment for SAM and MAM included the inadequacy of the quantity of RUTF (Ready to Use Therapeutic Food) and RUSF (Ready to use Supplementary Food) distributed to patients; failure to observe distribution of RUTF appointments; excessive consumption of other poor quality foods by the family including traditional complementary foods or boiled foods; use of traditional medicines and/or the administration of toxic herbs that affect appetite.
The three main indicators of the performance of the MAM patients and SAM outpatients are consistent with Spheres standards as several studies in Africa [25, 26]. Furthermore, the performance indicators for the recovered SAM without complications and MAM (87%) exceeded the recommended standards which are 75% [19]. The case study report of the CMAM in Tchad (Central Africa) noted that the outpatient nutrition center performance indicators were generally in agreement with the Sphere standards. Factors explaining this good performance include the availability and sufficiency of medicines, as well as strict application of the national protocol by health agents [27]. However, in our study centers, we reported failures to meet the standards. We assert that this could be addressed through regular training and supervision of MOH employed health officers.
The death rate in hospitalized SAM patients (33%) was higher than the recommended standard of 10%. In comparison to Gao pediatric hospital in Mali (West Africa), the death rate for SAM children was much lower at 12.3% [20]. Furthermore, in Bukavu (Democratic Republic of Congo) for the same period of five years, the death rate was only 7.5% [28]. Over five years in Burkina Faso, nutrition Centres reported a death rate of 16% again much lower than that observed in our study [29]. The poor outcome observed in our study could be attributed to the quality of care, lack of proper equipment, time pressures for doctors and nurses to undertake regular follow-up of hospitalized cases and a passive approach to screening by community health workers.
Analysis of the MUAC during the screening phase provided useful information about the status of the case and whether the child needed to be recruited for treatment. The existence of a large number of admissions with a low MUAC score was identified but the treatment was effective in that many cases reported an increased MUAC score during the treatment period.
In Burkina Faso, it is noted that CMAM support of a patient’s treatment costs USD 196.6 $ regardless of output (cured, death, default, and failure) [19]. In Benin, a similar project reported a much lower treatment cost of USD 164.45 $ per patient [30]. Whilst efficiencies in the delivery of the treatment could be explored further, a resource-effective approach could be to promote adequate supplementary feeding at the community level or focus on infant and young child feeding interventions which could be implemented in addition to CMAM and hence result in a lower cost as fewer patients would need the treatment.
In order to undertake treatment interventions at the health centers for malnourished children, close working cooperation between the two entities (MOH and NGOs) was essential. It was clear at the outset that the involvement of the members of the community, as well as the community health volunteer’s level, would be essential for the success of the program.
The compulsory community screening program enabled the identification of a high number of new cases that would potentially be undetected. Information from parents and caregivers indicates that they used traditional healers as the first line of treatment for a malnourished child. Late admissions of cases are associated with a higher risk of complications, longer treatment, increased abandonment of the program and a greater risk of adverse outcomes (including death). This, in turn, influences the perception of the program by the community and its uptake [31]. According to the case study of the CMAM in Chad (Central Africa), mothers brought malnourished children firstly to traditional healers; leaving the use of hospital care as the last resort [32]. Malnutrition is not really recognized as a disease, but rather mentioned through its signs and symptoms [19]. There is a need to address the ignorance about malnutrition and the recognition that effective treatment can be obtained at the community level and has a positive outcome if the disease is detected early.
The long distances for mothers, the low involvement of key people in the community, work overload in health center, RUTF and supplementary food stock breaks in some centers all constitute barriers to the accessibility and success of the intervention and treatment.
Parents also identified financial reasons as a barrier to seeking health center treatment of malnutrition in children. Some studies [33-38] recommend the free treatment of malnourished children in order to improve accessibility to the program, including the purchase of medicines. This was included in the program budget. The system of total exemption from payment for SAM inpatients throughout the district (ensured by the funders since 2012) was positively received by parents and nurses in the communities. This promoted attendance at medical centers when a child was referred.
The cost-free malnutrition program is essential because several pathologies were detected quicker and the survival of children was improved. The lack of communication between the parents/caregivers and the health workers on the cost-free malnutrition program could be a possible limitation.
The skills of community health workers were strengthened in relation to prevention, screening, awareness, sensitization, case referral, and community mobilization. However, the lack of collaboration and engagement with traditional healers and health workers was a possible barrier to the program. Improvement in communication and involvement in programs could increase the uptake of the treatments by the parents/caregiver.
The scaling up should be introduced gradually, with an anchorage certainly at the district level.
CONCLUSION
The program was successful in identifying and treating acutely malnourished children in the community who may otherwise not have received treatment. Despite this, the program failing to meet the Sphere standards for the duration of treatment and this research informs the direction needed to improve the situation. The cost-free aspect of this program was an incentive to undertake follow up treatment for parents of newly diagnosed cases and it is likely that treatment costs would be a barrier for the community. Thus, the challenge for Burkina Faso is how to ensure the sustainability of these efforts beyond the life of the program. Efforts to provide CMAM beyond the scope of the project should be developed with the involvement of all stakeholders.
It is important moving forward to ensure that CHW work with traditional healers to address the need for appropriate treatment and also that other infant and young child feeding practices are promoted at the community level which may address the prevention of MAM and SAM.
Without a balance between initial training, supervision, the organization of the nutritional inputs provided and sustainability, the scaling up may be compromised and become a burden for the existing health system.
Declarations
Ethics approval and consent to participate
The Regional Director of Health of MidWest had led the campaign in collaboration with the technical and financial partners. Mass awareness creation was made for the screening of acute malnutrition campaign in households. The objectives of the campaign were given. The consent of parents or legal guardians before any measurement was obtained. Severe acute malnourishment with complications detected children have been supported in health centers the same day.
The datasets used and analyzed during the current study are available from the corresponding author on a reasonable request.
Consent for publication
Not applicable
Availability of data and materials
All data generated or analyzed during this study are included in this published article
Funding
Supervision of processing of the SAM activities, a free support of all inpatient SAM cases, the strengthening of the capacities of health workers and community screening campaigns were funded from the European Union to the non-governmental Organization Lay Volunteer International Association (LVIA) and Medicus Mundi Italia (MMI).
ACKNOWLEDGMENTS
The funders are acknowledged for their support of this program, LVIA and MMI, which funded and supported action against severe acute malnutrition in the central west region. We acknowledge the support of the Regional Director of mid-west health and the health district of Reo for their collaboration in this work.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Ouédraogo Ousmane, Compaoré W. R. Ella, Philippe A. Nikiema and Virginio Pietra, conceived and designed the study. Ouédraogo Ousmane, Compaoré W. R. Ella, and Virginio Pietra, participated in data collection, and design of tables and analysis. Ouédraogo Ousmane, Compaoré W. R. Ella, Philippe A. Nikiema, Virginio Pietra and Ellahi Basma wrote and drafted the paper. Souho Tiatou and Ellahi Basma made the critical revision of the article. Final approval of the article was done by Amouzou Kou’santa Emile, Nicolas Meda, and Mamoudou H. DICKO.
REFERENCES