The common histopathological findings of colon biopsies in Northern Saudi Arabia
Fawaz D. Alshammri1*, Hussain Gadelkarim Ahmed2,3, Kalid Alshaghdali1, Hanan A. Oreiby4, Mohamed Ahmed B. Bealy2, Emad Abboh Abdallah Abboh2
1 Department of Clinical Laboratory, College of Applied Medical Science, University of Hail, Hail, Saudi Arabia.
2 College of Medicine, University of Hail, Hail, Saudi Arabia.
3 Department of Histopathology and Cytology, FMLS, University of Khartoum, Sudan.
4 King Khalid Hospital Hail, Saudi Arabia.
Email: fawazabof @ gmail.com
ABSTRACT
Background: Colorectal cancer is considered as the most prevalent cancer among men and the third most frequent cancer among women in Saudi Arabia. Consequently, we aimed to assess the common histopathological findings of colon biopsies in Northern Saudi Arabia. Methodology: This study has investigated the histopathological diagnosis of 88 patients subjected for colon and small intestine biopsies, their ages ranging from 18 to 99 years with a mean age of 48 years old at the Department of Pathology at King Khalid Hospital, Hail, Northern Saudi Arabia. Results: Out of the 88 patients, 53(60.2%) were males and 35(39.8%) were females. Diagnoses were reached in 77/88(87.5%) of the patients and could not be ascertained in 11/88(12.5%). Adenocarcinoma was diagnosed in 10/77(13%) of the patients (9/10(90%) in colon-site and 1/9(10%) in the small intestine. Conclusion: Colorectal precancerous and cancerous lesions are relatively prevalent among patients referred to colorectal diagnostic biopsy. There is a substantial percentage of inflammatory bowel cases among those referred to colorectal biopsies in Saudi Arabia.
Key words: Colorectal Cancer, Colon Biopsies, Histopathological Findings.
INTRODUCTION
Worldwide, colorectal cancer (CRC) represents the third most prevalent cancer with an overall increase of 60% resulting in the morbidity of over 2.2 million and mortality of over 1.1 million by the year 2030 [1]. The peak incidence rates are in Australia and New Zealand, Europe, and North America, and the lowermost rates are found in Africa and South-Central Asia [2].
Many causes were linked to the etiology of colon cancer. Demographic, behavioral and environmental factors were previously documented as risk factors for the development of CRC [3]. Patients over the age of 50 years represent more than 90% of the persons diagnosed with the disease.
Several reports have indicated the racial dissimilarities, particularly in cancer survivors, which might be linked to the pattern of CRC carcinoma (sporadic, inherited or familial). Around 70-75% of the patients are attending with sporadic types; hence, only 5-10% are attending with inherited type with their risk derived from hereditary or non-polyposis CRC. Patients with the history of colonic adenomatous polyps usually with a high risk of developing consequent CRC. Several components of diet and behavior have suggested being causes of CRC [4-12].
CRC is regarded as the most frequent cancer type among the male population and the 3rd utmost encountered cancer among the female population in Saudi Arabia [13]. In Saudi Arabia, the majority of patients with CRC attend with advanced stages of the disease, usually with metastasis, which makes the treatment challenging and increases the chance of death [14]. In recent years, there has been a trend toward colorectal cancer awareness and screening in Saudi Arabia, which has facilitated the detection of many cases [15]. Therefore, the present study aimed to assess the common histopathological findings of colon biopsies in Northern Saudi Arabia.
MATERIALS AND METHODS
In the present study, the data regarding colorectal biopsies were retrieved from the Department of Pathology at King Khalid Hospital, Hail, Northern Saudi Arabia. The data referring to colorectal biopsies patients who were diagnosed during the period from January 2018 to December 2018 were included. The diagnosis of colorectal lesion was confirmed by conventional histopathology. The re-evaluation of the histopathological diagnosis of the tissue samples was completed to confirm the prior diagnosis and to categorize the classification of the lesions into benign and malignant types.
Statistical analysis:
The obtained information sets were entered into a computer software; Statistical Package for Social Sciences (SPSS version 16; SPSS Inc, Chicago, IL). Chi-square test was and P < 0.05 was considered significant.
Ethical consent:
The protocol of this study was established agreeing with the 2013 Declaration of Helsinki and this study was approved by the ethics committee of the College of Medicine, University of Hail, Saudi Arabia. Ethical Committee approval number was EC00069.
RESULTS
The present study explored the histopathological diagnosis of 88 patients subjected for colon and small intestine biopsies, their ages ranging from 18 to 99 years with a mean age of 48 years old. Out of the 88 patients, 53(60.2%) were males and 35(39.8%) were females. The majority of patients were found at age group ≤30 years followed by ≥61, and 51-60 years old representing 24/88(27.3%), 23/88(26.1%) and 17/88(19.3%), respectively. Most males were found in the age range ≥61years followed by ≤30 years, and 51-60 years constituting 15/53(28.3%), 12/53(22.6%), and 11/53(20.7%), in this order. Most females were noticed at the age group ≤30 years followed by ≥61, and 51-60 years representing 12/35(34.3%), 8/35(22.8%), and 6/35(17%), correspondingly, as indicated in Table 1. Fig 1.
Table 1. Distribution of the patients by sex and age
|
Age group |
Males |
Females |
Total |
|
≤30 years |
12 |
12 |
24 |
|
31-40 |
8 |
5 |
13 |
|
41-50 |
7 |
4 |
11 |
|
51-60 |
11 |
6 |
17 |
|
≥61 |
15 |
8 |
23 |
|
Total |
53 |
35 |
88 |
Figure 1. Description of the patients by sex and age
Specific initial clinical presentations were available for 44/88(50%) of the patients.
Table 2 summarized the distribution of the patients by initial clinical findings and biopsy site. The majority of patients (both sex) presented with rectal polyps followed by the clinical presentation of ulcerative colitis or IBS representing 24/44(54.5%) and 11/44(25%) in this order. The highest frequent biopsy site was colon followed by the small intestine, and rectum constituting 40/88(45.5%), 23/88(26%) and 20/88(23%), in this order, as shown in Fig 2.
Table 2. Distribution of the patients by initial clinical findings and biopsy site
|
Variable |
Males |
Females |
Total |
|
initial clinical findings |
|
|
|
|
Rectal polyp |
15 |
9 |
24 |
|
Perianal fistula |
3 |
0 |
3 |
|
Ulcer |
1 |
2 |
3 |
|
Ulcerative colitis or IBS |
5 |
6 |
11 |
|
Celiac disease |
2 |
0 |
2 |
|
H. Pylori |
0 |
1 |
1 |
|
Total |
26 |
18 |
44 |
|
Undefined |
27 |
17 |
44 |
|
Biopsy site |
|
|
|
|
Rectum |
12 |
8 |
20 |
|
Anus |
4 |
1 |
5 |
|
Colon |
22 |
18 |
40 |
|
Small intestine |
15 |
8 |
23 |
|
Total |
53 |
35 |
88 |
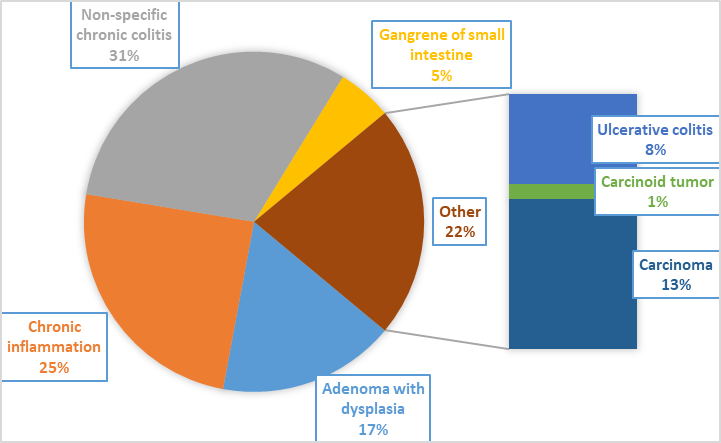
Figure 2. Description of the patients by initial clinical findings and biopsy site
Table 3 summarized the distribution of the patients by sex and histopathological diagnosis. Diagnoses were reached in 77/88(87.5%) of the patients and could not be ascertained in 11/88(12.5%). Adenocarcinoma was diagnosed in 10/77(13%) of the patients (9/10(90%) in colon-site and 1/9(10%) in the small intestine. Out of 10 carcinoma cases, 7/10(70%) occurred in males and 3/10(30%) in females, the risk of colon cancer was found to be statistically significant among males P < 0.0001. Adenoma was identified in 13/77(%) of whom 6/45(13%) were males and 7/32(22%) females. Adenoma was more common among females compared to females and this was found to be statistically significant (P <0.05). Chronic inflammation was diagnosed in 19 patients (13 were males and 6 were females). Chronic inflammation was significantly associated with male gender. Non-specific chronic colitis was identified in 24 patients (13 were males and 11 were females) as shown in Figures 3 and 4, and Photos 1, 2, and 3.
Table 3. Distribution of the patients by sex and histopathological diagnosis
|
Diagnosis |
Males |
Females |
Total |
|
Adenoma with dysplasia |
6 |
7 |
13 |
|
Chronic inflammation |
13 |
6 |
19 |
|
Non-specific chronic colitis |
13 |
11 |
24 |
|
Gangrene of small intestine |
2 |
2 |
4 |
|
Ulcerative colitis |
3 |
3 |
6 |
|
Carcinoid tumor |
1 |
0 |
1 |
|
Carcinoma |
7 |
3 |
10 |
|
Total |
45 |
32 |
77 |
|
Undefined diagnosis |
8 |
3 |
11 |
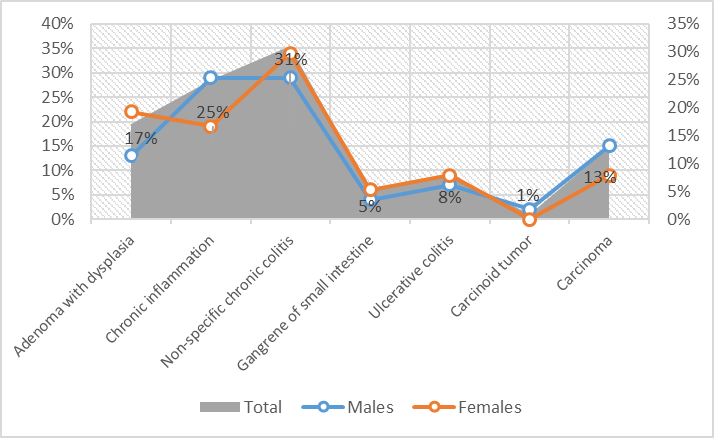
Figure 3. Proportions of diagnosis among patients
Figure 4. The patients by sex and histopathological diagnosis
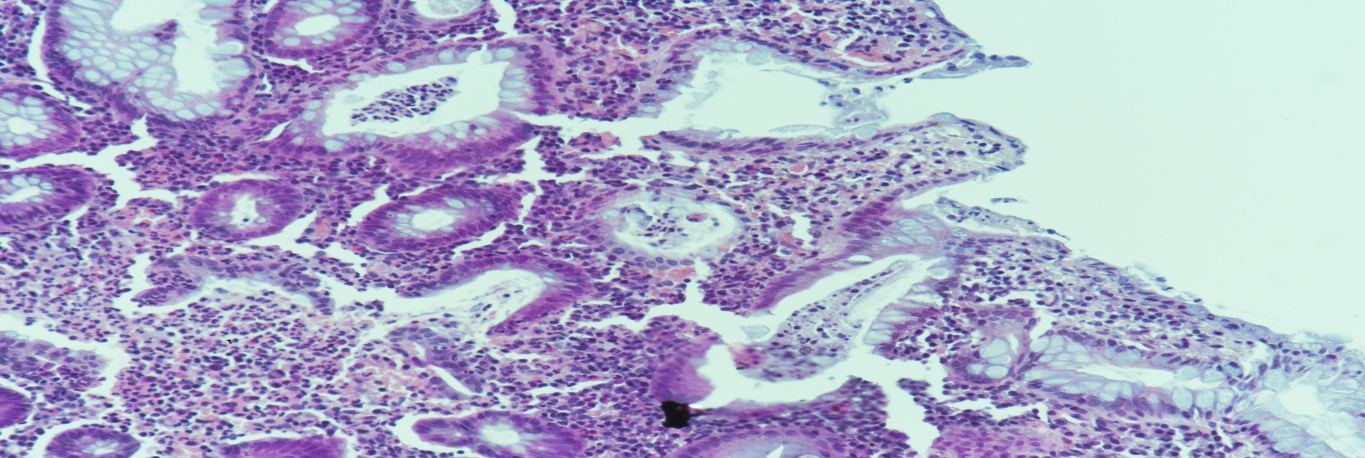
Photo 1. Large bowel: Hematoxylin and Eosin (H & E) (X100): Ulcerative colitis
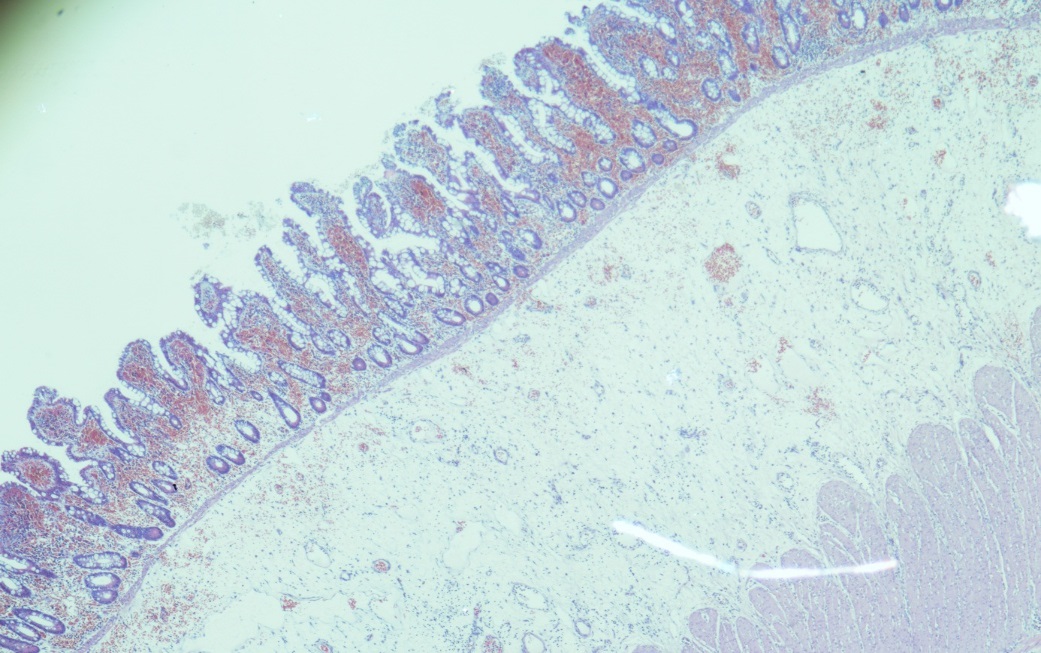
Photo 2. (H & E 40): Small bowel gangrene: showing necrosis of mucosal epithelium, inflammation, and hemorrhage
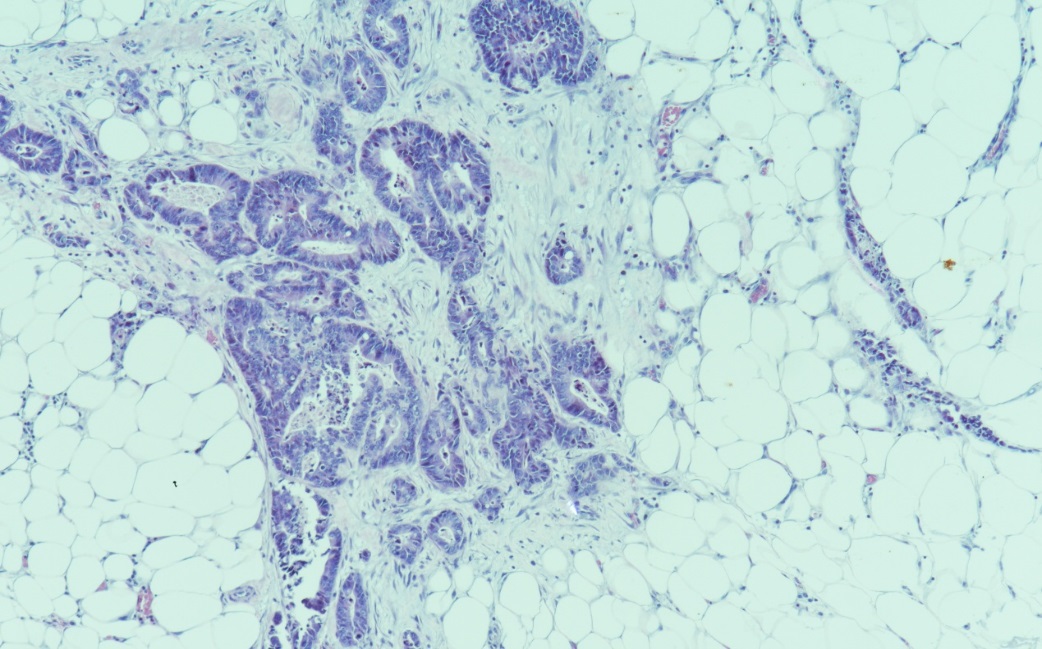
Photo 3. (H & E 40): Moderately adenocarcinoma with high nuclear grade and invasion of pericolic fat
Table 4 summarized the distribution of the patients by age and histopathological diagnosis. Most of the cases of carcinomas were found in the age range of 41-60 years (7/10(70%)). Most of the cases of adenomas were found in the age range of 51+ years (10/13(77%)). Most cases of nonspecific chronic colitis were identified in the age group ≤30years followed by ≥61 years representing 11/24(46%) and 7/24(29%) in this order, as shown in Fig 5.
Table 4. Distribution of the patients by age and histopathological diagnosis
|
Diagnosis |
≤30years |
31-40 |
41-50 |
51-60 |
≥61 |
Total |
|
|
|
|
|
|
|
|
|
Adenoma with dysplasia |
0 |
2 |
1 |
5 |
5 |
13 |
|
Chronic inflammation |
4 |
5 |
2 |
2 |
6 |
19 |
|
Non-specific chronic colitis |
11 |
0 |
1 |
4 |
7 |
24 |
|
Gangrene of small intestine |
1 |
1 |
0 |
0 |
2 |
4 |
|
Ulcerative colitis |
3 |
3 |
0 |
0 |
0 |
6 |
|
Carcinoid tumor |
0 |
0 |
0 |
1 |
0 |
1 |
|
Carcinoma |
1 |
0 |
4 |
3 |
2 |
10 |
|
Total |
20 |
11 |
9 |
15 |
22 |
77 |
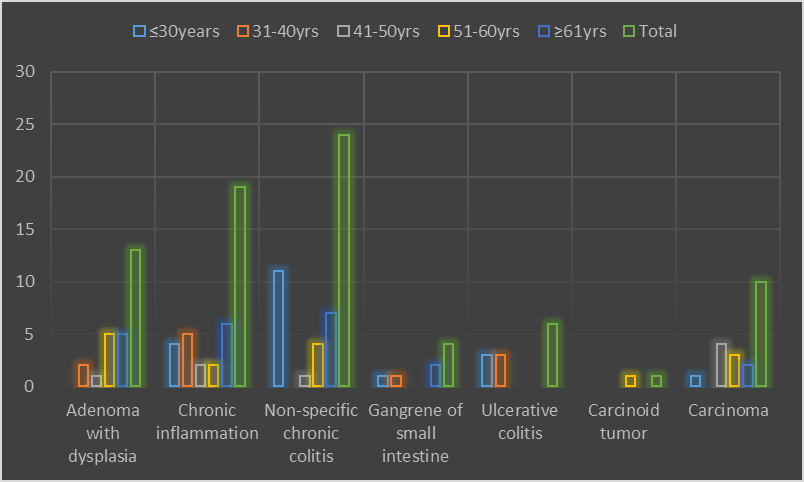
Figure 5. Age by histopathological diagnosis
DISCUSSION
The present study investigated a full coverage of colorectal biopsies obtained within one year in Northern Saudi Arabia. The majority of patients were males with older age. CRC was recognized in 11/88(12.5%) of the patients most of them were males and premalignant conditions were identified in 13/88(14.8%) with females greater than males. Although there was an insufficiency of information in this regard, relatively similar findings were earlier informed from Saudi Arabia. CRC was considered as the most common males’ cancer and the 3rd mutual females’ cancer since 2002 in the country. There has been a minor preponderance stuck between men with an average ratio of 116:100 over the years (range: 99:100–132:100). The overall age-standardized rate (ASR) come near a plateau of 9.6/100 000 in 2010 [16].
A reasonable number of patients with colorectal patients were seen at a relatively younger age <50 years old. Although many investigations have revealed that the risk of colon cancer increases after the age of 50 years [17, 18], a study from Saudi Arabia has reported that CRC occurs at an earlier age in Saudis, particularly among females. This has the most important suggestion for choices about the threshold age for screening. The ASR has been increased yet greatly lower than in the developed world. Factors lying behind the decreased survival in developing countries include shortage or absence of screening, increasing of cases diagnosed with advanced stages of the disease, lack of sufficient medical care in rural areas and the escalating incidence of CRC cases [16].
In the present study, chronic inflammation and non-specific colitis of the colon were diagnosed in 25% and 31% of the patients, respectively. The inflammatory bowel diseases (IBD), comprising Crohn's disease (CD) and ulcerative colitis (UC), are chronic inflammatory disorders of the intestine [19]. A study from Saudi Arabia reported that in a total of 312 of the cases with IBD, included 63% of the cases with CD and 37% of the cases with UC. In Saudi Arabia, the epidemiology, clinical characteristics, and natural course of IBD are still generally unidentified [20].
In the current study, UC was found in 8% of the patients. A study from Saudi Arabia has reported that the bulk of UC patients were younger aged individuals (17-40 years), with men being dominant. Whereas the disease course was instituted to be alike to that described in the Western world, additional resemblances were reported with Asian nations regarding the magnitude of the disease and response to steroid therapy. Despite some studies proposing an upsurge in the occurrence of UC in the Arabian nation in the latest years, there is a deficient evidence about it, mainly in Saudi Arabia [21].
CONCLUSION
Colorectal precancerous and cancerous lesions are relatively prevalent among patients referred to colorectal diagnostic biopsy. There is a significant percentage of inflammatory bowel cases among those referred to colorectal biopsies in Saudi Arabia.
ACKNOWLEDGMENT
The author would like to thank people at the Department of Pathology at King Khalid Hospital for their help and cooperation in data collection.
REFERENCES